UTHealth Houston receives $3.4 million in grants for trauma research initiatives
Groundbreaking research initiatives to advance the treatment of traumatic injuries at UTHealth Houston have been funded with $3.4 million in grants from the Trauma Research and Combat Casualty Collaborative (TRC4), an initiative of The University of Texas System.
“These research awards from UT System are a testament to the amazing work of our McGovern Medical School faculty and will ultimately improve the care and outcomes for trauma patients,” said executive dean John Hancock, MA, MB, BChir, PhD, ScD, who holds the H. Wayne Hightower Distinguished Professorship in the Medical Sciences and the John S. Dunn Distinguished University Chair in Physiology and Medicine.
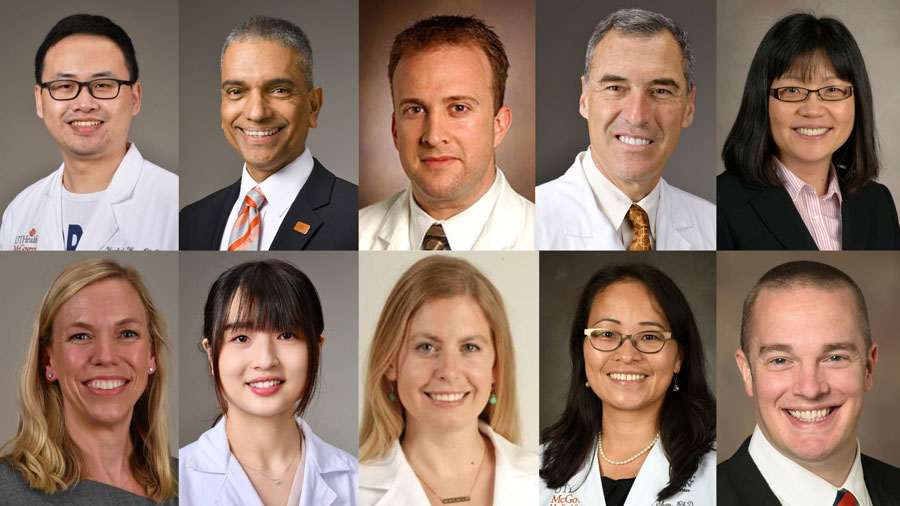
Ten researchers received grants for research encompassing diverse focus areas, from liver and traumatic brain injuries to blood clot prevention, pediatric blood vessel injuries, and spinal cord recovery:
The role of white blood cells in traumatic liver injuries: Yankai Wen, PhD, instructor in the Department of Anesthesiology, Critical Care and Pain Medicine, will focus his research on the impact of hypoxia-inducible factor 1-alpha (HIF1α) in patients who have sustained traumatic liver injuries. By examining how neutrophils, a type of white blood cell, respond to low oxygen levels during these injuries, Wen and his team will aim to uncover the potential effects of HIF1α. This deeper understanding of the process could not only help patients with traumatic liver injuries recover more fully, but also significantly advance the field of liver injuries and treatment, opening new avenues for innovative approaches.
Understanding the impact of traumatic brain injuries (TBI) in senior citizens and possible links to neurodegenerative disorders: Some studies suggest that older adults without cognitive issues have an accumulation of a protein called beta-amyloid in the brain, which is often associated with Alzheimer’s disease and other neurodegenerative disorders. Currently, researchers don’t know if the presence of the protein worsens the consequences of a TBI. Pramod Dash, PhD, will examine if reducing brain beta-amyloid load would improve outcomes for older people who sustain concussions. Dash is a professor and chair of the Department of Neurobiology and Anatomy and the Nina and Michael Zilkha Distinguished Chair in Neurodegenerative Disease Research. He is also a member of The University of Texas MD Anderson Cancer Center UTHealth Houston Graduate School of Biomedical Sciences.
Unlocking the potential of using green plasma: Over the past 20 years, the use of plasma in trauma patients has increased. However, the amount of plasma donated doesn’t meet the current demand. Plasma donated by pregnant women or those taking birth control pills often looks green, so it is frequently discarded even though there is no evidence that it is harmful or not useable. Bryan Cotton, MD, MPH, John B. Holmes Professor in the Clinical Sciences and director of the Surgical Critical Care Fellowship in the Department of Surgery, will examine the potential promise green plasma may hold in treating excessive bleeding.
Unraveling how genes affect brain swelling after traumatic injury: Charles S. Cox, Jr., MD, will investigate the influence of specific genes, known as SUR1/TRMP4 polymorphisms, and their potential to mitigate brain damage in patients who have suffered head trauma. Swiftly identifying these differences within four hours of an injury could allow physicians to tailor treatment, potentially enhancing a patient’s chances of survival. In a novel approach, Cox and his team will also explore the use of freeze-dried particles made from substances produced by stem cells. These stem cells are grown in a container known as a bioreactor, which encourages them to release proteins that reduce inflammation. The innovative use of these proteins could revolutionize the treatment of brain injuries by significantly decreasing swelling and inflammation in the brain after an injury. Cox, professor of pediatric surgery, is the George and Cynthia Mitchell Distinguished Chair in Neurosciences, Glassell Family Distinguished Chair, and director of the Pediatric Translational Laboratories and Program in Children’s Regenerative Medicine. He is also a member of MD Anderson Cancer Center UTHealth Houston Graduate School of Biomedical Sciences.
Exploring new ways to treat severe liver injuries by harnessing white blood cells to speed healing: Damage to the liver sustained during accidents or wartime situations has traditionally been challenging to treat. Previous research has shown that a type of white blood cell known as eosinophils might help protect the liver after trauma. Cynthia Ju, PhD, professor and Joseph C. Gabel, MD, Endowed Chair in Anesthesiology, will grow eosinophils from cord blood to determine if the white blood cells reduce liver damage and accelerate healing, leading to novel ways of treating severe liver injuries.
Advancing the management and treatment of pediatric blood vessel injuries: As firearm incidents continue to rise, so do pediatric blood vessel injuries, which are complicated to treat. Multicenter databases have greatly enhanced data collection for adult cases; however, obtaining meaningful data for pediatric patients poses challenges. Natalie Drucker, MD, MS, surgical critical care fellow and staff physician in the Department of Pediatric Surgery, and her team will create a dedicated pediatric registry providing essential data for informed decision-making and improving care for children who sustain these life-threatening injuries. The pediatric database will eventually be merged with the adult database, increasing treatment options and approaches.
Investigating how white blood cells aid in the recovery of patients with traumatic liver injuries: When the liver is injured and experiences a lack of blood flow, it releases a substance known as IL-33, activating a type of white blood cell known as eosinophils that plays a role in the body’s immune system response. Yang Yang, PhD, instructor in the Department of Anesthesiology, Critical Care and Pain Medicine, will further study eosinophils and how they protect the liver after a patient sustains life-threatening injuries.
Exploring the use of statins for blood clots: Blood clots remain a severe complication for patients with life-threatening injuries, increasing the risk of death. Gabrielle Hatton, MD, acute care surgery fellow and staff physician in the Department of Surgery, will conduct an observational study that will strive to uncover further evidence that statins, drugs routinely prescribed for high cholesterol, could be used to treat blood clots. She and her team will collect blood samples from patients and compare blood vessel function markers and blood clot rates in patients who do or do not take a regularly prescribed statin. They also will interview physicians and patients to better understand their experiences with standard blood clot prevention methods and their willingness to take a statin if it reduces the risk of blood clots after injury.
Protecting kidneys after traumatic injuries using proton pump inhibitors (PPIs): Kidney failure is common after a traumatic injury and is one of the primary reasons why patients don’t survive. If they do survive, kidney issues can lead to long-term complications, resulting in long hospital stays and increased health care costs. Previous research has indicated that PPIs, commonly prescribed for acid reflux, may help protect the kidneys. Yafen Liang, MD, associate professor and chief of the Division of Cardiovascular Anesthesiology in the Department of Anesthesiology, Critical Care and Pain Medicine, and Memorial Hermann Chair, will take the research one step further to determine if administrating PPIs intravenously can prevent kidney problems in trauma patients, potentially saving more lives.
Determining the most effective strategy for blood pressure management after spinal cord injuries: David E. Meyer, MD, MS, assistant professor in the Department of Surgery, will delve into the most effective ways to manage blood pressure to improve blood flow to the spinal cord after traumatic spinal cord injury. The study will focus primarily on recovery. Meyer’s research will assess a patient’s ability to move, feel sensations, and perform everyday tasks at six weeks, six months, and one year after injury. By examining various strategies for managing blood pressure and intraspinal pressure, Meyer and his team aim to identify interventions that hold promise of enhancing patients’ quality of life and functional abilities over time.
UTHealth Houston, in collaboration with The University of Texas Health Science Center at San Antonio and The University of Texas at Tyler, was also awarded two other significant grants totaling $1.5 million to advance research in critical areas of trauma.
The first grant of $500,000 will fund research to identify genetic factors that influence the extent of brain swelling following traumatic brain injury. By identifying specific genetic variations, researchers hope to develop more personalized treatment strategies to improve patient outcomes. The second grant, totaling $1 million, will support the iRemedyACT project, which focuses on identifying and addressing delays in providing definitive care to critically injured patients within the Texas Trauma System.