Research reveals ‘big picture’ of perioperative organ injury
After nearly four years researching the surgical outcomes of more than 28 million patients, McGovern Medical School investigators are illuminating the global impact of perioperative organ injury.
Findings from “Impact of Peri-operative Organ Injury on Morbidity and Mortality in 28 Million Surgical Patients,” published online in Nature Communications April 9, indicate that perioperative mortality is the third-leading cause of death.
The perioperative period has been referred to as the “neglected stepchild of global health,” wrote the authors. “Our findings will help create therapeutic strategies to improve perioperative outcomes,” said Yafen Liang, MD, study author, professor of anesthesiology and Memorial Hermann Chair.
Despite advances in anesthesia and surgical techniques, significant morbidity and mortality still occur following surgery. A recent modeling study estimated that 234 million major surgeries are performed each year, with up to 4 percent of patients predicted to die during that hospitalization. In addition, up to 15 percent experience severe postoperative morbidity, amounting to an estimated 1,000 deaths and 4,000 major complications every hour.
“Anesthesia has become extremely safe; however, patients still die during this perioperative period following surgery because of organ failure,” said Liang, adding that perioperative organ injury can be exacerbated by co-morbidities and essentially affect every organ system.
To improve therapeutic strategies and surgical outcomes, researchers with the Department of Anesthesia, Critical Care and Pain Management, and colleagues, accessed surgical data from all elective and emergent surgeries between 2014-17 from the German Federal Statistics Office.
“In Germany, it’s a bit different – every surgical case has to be recorded and submitted with very detailed information so that the hospital can be reimbursed,” explained Liang, the department’s vice chair of clinical research and chief of the Division of Cardiovascular Anesthesiology.
Using traditional and comprehensive statical analysis, researchers found that in-hospital mortality was 1.4 percent, and 4.4 percent of cases experienced perioperative organ injury. Perioperative organ injury was associated with a nine-times higher odds of death and prolonged hospital stay.
“Previous papers only looked at specific patient population, like cardiac surgery patients,” Yafen said. “It’s rare for a study with such a large patient population to look at individual organ injury, so we know what is more and less important – incidence rate and mortality – to prioritize our efforts.”
Investigators found the highest organ injury incidence rate was the kidneys, at 2 percent, which was associated with one-quarter of the mortalities. The second-highest incidence, delirium at 1.5 percent, was associated with the lowest mortality, 10.8 percent. This was followed by acute myocardial infarction (.6 percent incidence, 15.6 percent mortality), stroke (.6 percent incidence and 13.1 percent mortality), pulmonary embolism (.3 percent incidence and 20 percent mortality), liver injury (.1 percent incidence and 68.7 percent mortality), and acute respiratory distress syndrome (.1 percent incidence and 44.7 percent mortality).
“This paper looks at the impact of individual organ injury, which are the most important ones, as well as concurrent organ injury following surgery. Looking at them together gives us a big picture of organ injury,” she said.
Yafen said it was enlightening to see the immense impact of perioperative organ failure, which she said will be of public health interest to epidemiologists, policymakers, and the general public, Yafen added.
“We definitely want to do follow-up studies to dive in-depth to see what these outcomes mean for certain patient populations, by age, sex, or the effects of obesity,” she said.
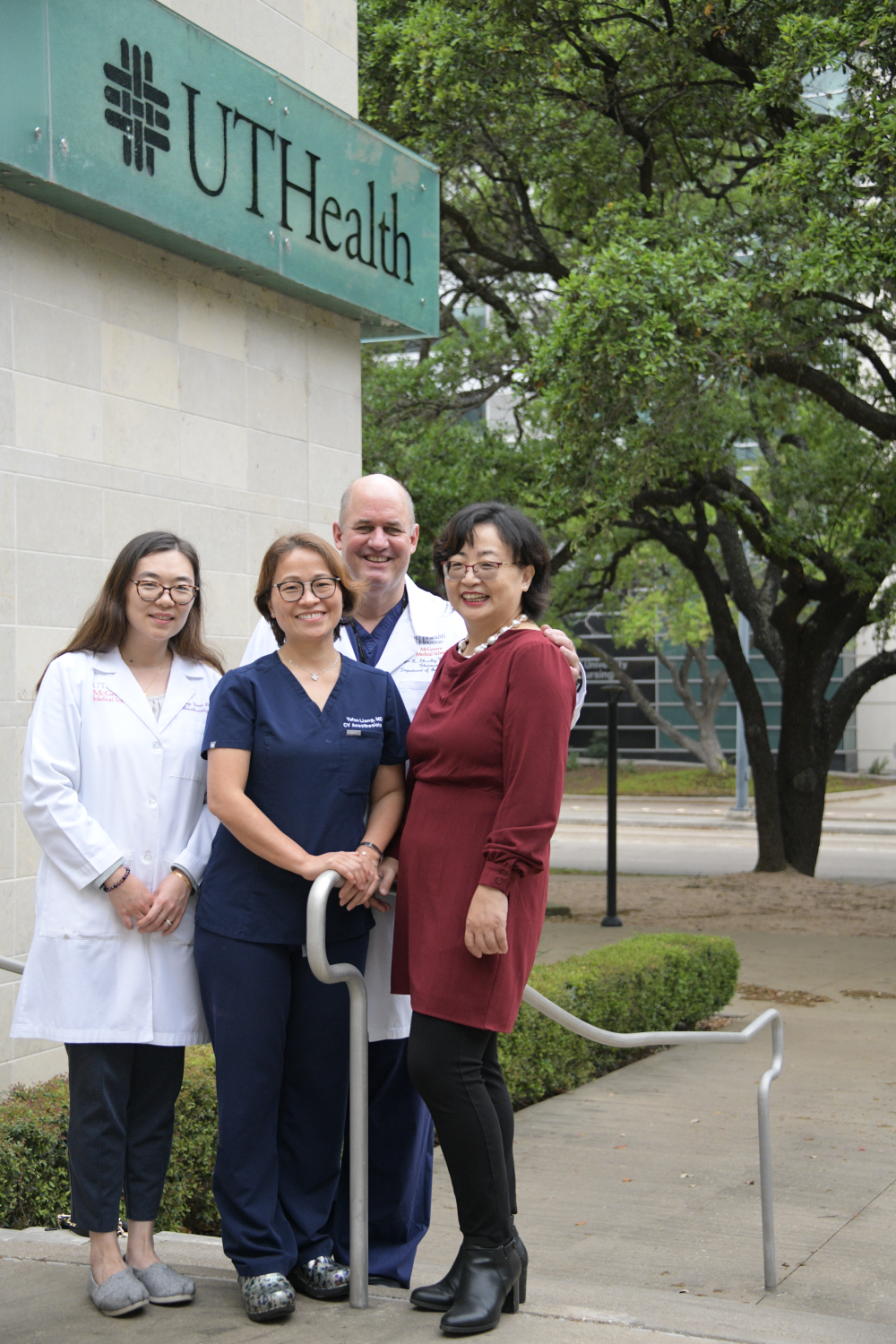
Additional collaborators from UTHealth Houston include Xiaoyi Yuan, PhD, and Holger Eltzschig, MD, PhD, Department of Anesthesia, Critical Care and Pain Medicine, and Hongfang Liu, PhD, McWilliams School of Biomedical Informatics. Collaborators also include Felix Kork, MD, MSc, and Rolf Rossaint, MD; RWTH Aachen University, Germany; Adit Ginde, MD, MPH, University of Colorado School of Medicine; and Alex Evers, MD, Washington University School of Medicine in St. Louis.