Pediatric Neuroscience Journal – Fall 2023
Toward Better Lives for All Children
Among the comments made by Nelson Mandela in a 2002 address delivered to the United Nations is a sentence that has great meaning for us: “History will judge us by the difference we make in the everyday lives of children.” Every decision we make as faculty at McGovern Medical School at UTHealth Houston is guided by that principle. Our clinician team is very aware that a single decision can change a patient’s future, that our research has the potential to advance medicine, and that our beliefs and attitudes are passed on to the physicians we train. For these reasons, we foster collaboration among physicians, scientists, nurses, therapists, and other health care professionals. Everyone brings something unique and important to the table.
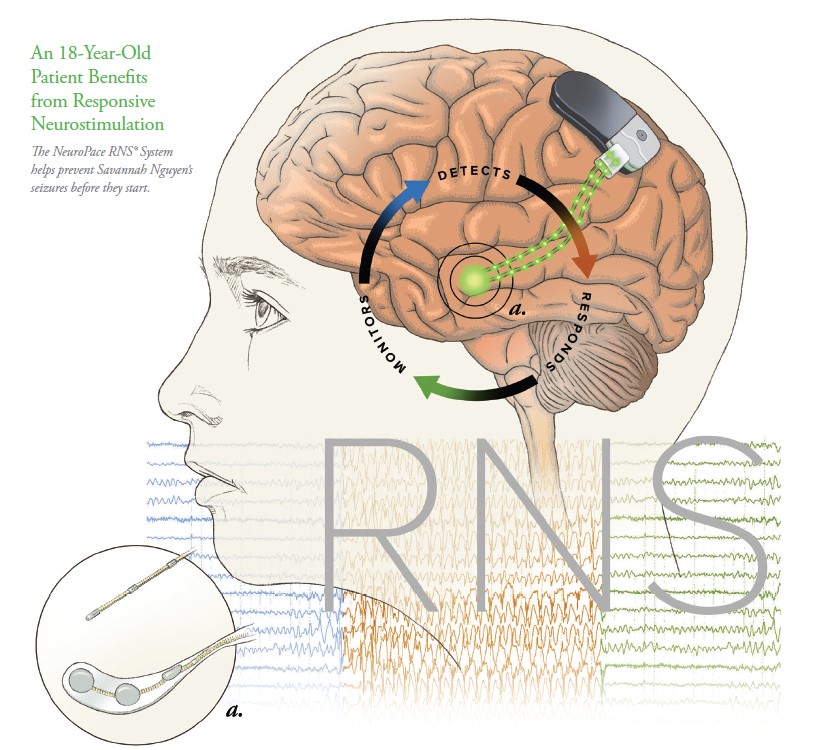 The three patients we highlight in this issue were selected because they’re making remarkable progress toward full lives despite the challenges they face. Eighteen-year-old Savannah Nguyen suffered uncontrolled tonic-clonic seizures for seven years before her family came to UTHealth Houston for treatment. Responsive neurostimulation using the NeuroPace RNS® System has decreased her seizure burden by more than 60% to date, with continued improvement with every increase in stimulation.
The three patients we highlight in this issue were selected because they’re making remarkable progress toward full lives despite the challenges they face. Eighteen-year-old Savannah Nguyen suffered uncontrolled tonic-clonic seizures for seven years before her family came to UTHealth Houston for treatment. Responsive neurostimulation using the NeuroPace RNS® System has decreased her seizure burden by more than 60% to date, with continued improvement with every increase in stimulation.
Te’Niyah Lane suffered a brain hemorrhage at birth and after intubation and CPR in Labor & Delivery was admitted to the hospital’s Level IV NICU. She left the NICU 43 days later with an appointment scheduled at the hospital’s NICU Follow-Up Clinic, where a multidisciplinary team delivers coordinated care that means earlier recognition of problems and ultimately, better outcomes. Bryan Rowley arrived in the hospital’s Level 1 Pediatric Trauma Center with an ear infection that had spread to the bone of his skull, causing a cerebral venous thrombosis. His physician team successfully chose a combination of medications and watchful waiting, avoiding neurosurgery to place a ventriculoperitoneal shunt.
You will also read about exciting research under way in the Pediatric Neurology Clinical Research Program; the successful results of a feasibility study for fetoscopic myelomeningocele repair using a novel human umbilical cord patch; a laboratory model of intraventricular hemorrhage (IVH) that simulates different stages of brain development in preterm infants – the first data to show that the outcome of IVH is dependent on brain development, suggesting that post-hemorrhagic hydrocephalus depends on inflammation that occurs as the brain develops; and ongoing studies to improve outcomes in children with malignant fourth ventricular brain tumors.
We hope you find the articles in this issue of the Pediatric Neuroscience Journal useful in your practice – and that they prompt you to look at your patients in new ways. If you have questions about any of our programs, please contact us directly.
Inside this Edition:
- Responsive Neurostimulation for Generalized Epilepsy in an 18-Year-Old
- The NICU Follow-Up Clinic: Everything Premature Babies Need To Get the Best Start in Life
- Team-Based Medicine Leads to Nonsurgical Repair of Depressed Skull Fractures in Two Neonates
- Watchful Waiting for Cerebral Venous Thrombosis Allows a Boy To Avoid Brain Surgery
- UTHealth Houston Team Completes Feasibility Study for Minimally Invasive Myelomeningocele Repair in 25 Patients
- Developing Better Laboratory Models of Neonatal Intraventricular Hemorrhage and Hydrocephalus
- Researchers Seek to Improve Outcomes in Children with Malignant Fourth Ventricular Brain Tumors Through Novel Studies
- McGovern Medical School Alumni Blend Neurology Expertise and Philanthropy To Advance Pediatric Tumor Research
With best wishes,
David I. Sandberg, MD, FAANS, FACS, FAAP
Professor and Director of Pediatric Neurosurgery
Dr. Marnie Rose Professor in Pediatric Neurosurgery
THINK Neurology Chair in Pediatric Tumor Research and Innovation
Department of Pediatric Surgery and Vivian L. Smith Department of Neurosurgery
McGovern Medical School at UTHealth Houston and Children’s Memorial
Hermann Hospital
Co-director, Pediatric Brain Tumor Program
The University of Texas MD Anderson Cancer Center
Gretchen Von Allmen, MD
Professor of Pediatrics and the Jacobo Geissler Distinguished
Chair in West Syndrome Research
Director, Pediatric Epilepsy Program
Division Director, Child and Adolescent Neurology
Co-Director, West Syndrome Center of Excellence
McGovern Medical School at UTHealth Houston
Medical Director, Pediatric Epilepsy Monitoring Unit
Children’s Memorial Hermann Hospital











