Team-Based Medicine Leads to Nonsurgical Repair of Depressed Skull Fractures in Two Neonates
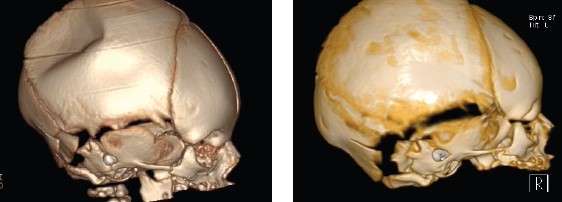
A depressed skull fracture in a newborn – also called a ping-pong fracture – is a rare diagnosis that usually requires general anesthesia, an open craniotomy, and the use of various surgical instruments to correct the defect.
The pediatric neurosurgery team at McGovern Medical School at UTHealth Houston put their heads together and came up with an elegantly simple solution using an object commonly found in Neonatal Intensive Care Units – a breast pump.
“If you squeeze a ping-pong ball, there’s no true break but there is a significant indentation,” says Emilie L. Martinez, MS, PA-C, a physician assistant and the advanced care provider coordinator in the Division of Pediatric Neurosurgery at McGovern Medical School.
“We were caring for a neonate with a ping-pong fracture in our NICU. At one of our pediatric neurosurgery team conferences, we discussed a similar case reported in a neurosurgical journal in which an obstetrics vacuum, an assistive device that applies suction and traction to help babies move through the birth canal, was used to pop the indentation out. We did not have an obstetric pump easily available for use and were concerned that the amount of suction might injure the neonate.”
A new mother herself, Martinez thought about adapting a breast pump for repair of the depressed skull fracture. She ran the idea by David Sandberg, MD, FAANS, FACS, FAAP, professor and director of pediatric neurosurgery, Dr. Marnie Rose Professor in Pediatric Neurosurgery, and THINK Neurology Chair in Pediatric Tumor Research and Innovation, who encouraged her to develop her idea further. She met with a hospital lactation consultant to explore how a breast pump could be adapted for use on the newborn’s skull and used Coloplast® – a moldable adherent utilized to fit ostomy bags – to custom fabricate a mold to fit the breast pump flange to the infant’s skull.
In two cases of depressed skull fracture in the hospital’s NICU – the first in June 2021 and later in September 2022 – the families were willing to try the innovative procedure to avoid skull surgery. “Dr. Sandberg and I went to the NICU, turned on the pump, and within a few minutes, the suction gently popped the newborn’s skull back into place,” says Martinez, who is submitting an article about the technique for publication. “This is a great example of the power of team-based medicine. It’s about using devices and materials readily available in the hospital and applying each person’s expertise to arrive at a beautifully simple and novel solution. We want to share our experience in the hope that it will help other families.”
Inside this Edition:
- Responsive Neurostimulation for Generalized Epilepsy in an 18-Year-Old
- The NICU Follow-Up Clinic: Everything Premature Babies Need To Get the Best Start in Life
- Team-Based Medicine Leads to Nonsurgical Repair of Depressed Skull Fractures in Two Neonates
- Watchful Waiting for Cerebral Venous Thrombosis Allows a Boy To Avoid Brain Surgery
- UTHealth Houston Team Completes Feasibility Study for Minimally Invasive Myelomeningocele Repair in 25 Patients
- Developing Better Laboratory Models of Neonatal Intraventricular Hemorrhage and Hydrocephalus
- Researchers Seek to Improve Outcomes in Children with Malignant Fourth Ventricular Brain Tumors Through Novel Studies
- McGovern Medical School Alumni Blend Neurology Expertise and Philanthropy To Advance Pediatric Tumor Research











