Watchful Waiting for Cerebral Venous Thrombosis Allows a Boy to Avoid Brain Surgery
In January 2021 at the age of 3, Bryan Rowley was still nonverbal and diagnosed by a neurologist in Galveston with mild autism spectrum disorder (ASD). By late March of that year he had turned 4 and was in and out of the hospital for more than a month with a persistent ear infection diagnosed as a virus.
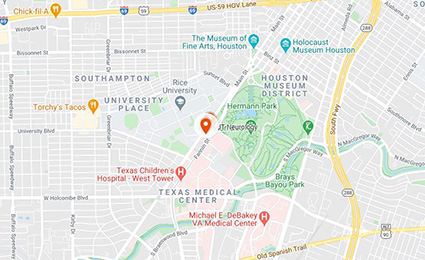
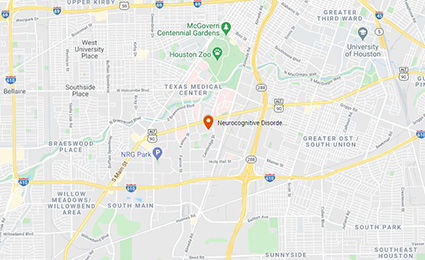
Finally his mother, Gabriela Blanco, a nurse who lives in Galveston County, took him to the emergency department. “By the time he came under our care, Bryan’s ear infection had spread to the bone of his skull and caused a blood clot in his right jugular vein,” says Stuart Fraser, MD, director of the Program for Pediatric Stroke and Cerebrovascular Disease at the Institute for Stroke and Cerebrovascular Disease at UTHealth Houston and an assistant professor of pediatric neurology at McGovern Medical School. “The clot interfered with normal drainage of blood from Bryan’s head, causing cerebral venous thrombosis (CVT) and elevated intracranial pressure (ICP). Left untreated, CVT can lead to brain bleeding and stroke.”

Bryan Rowley, diagnosed with cerebral venous thrombosis, is thriving after a team of specialists used medication and watchful waiting to avoid surgery.
An uncommon disorder, CVT can manifest as headache, visual loss, focal or generalized seizures, neurologic deficits, confusion, and coma. The seriousness of the condition led Fraser and Manish N. Shah, MD, FAANS, to consider ventriculoperitoneal shunting to relieve ICP caused by fluid buildup. Shah is the William J. Devane Distinguished Professor and associate professor of pediatric neurosurgery at the medical school, director of pediatric epilepsy surgery, and director of the Texas Comprehensive Spasticity Center at UTHealth Houston Neurosciences.
But instead of moving forward with surgery, in conference with Bryan’s physician team and his family, Fraser and Shah decided on a more conservative approach, using blood thinners to prevent stroke and Diamox® to decrease fluid production and pressure in the brain.
“This approach worked for Bryan, but we knew we couldn’t keep him on medication forever. He had a very small transverse vein on the left and we were betting that we could buy him enough time so that the left side would enlarge as he grew,” Fraser says.
Bryan was hospitalized at Children’s Memorial Hermann Hospital for about three weeks. In addition to the care he received at the hospital, Blanco, who was then working as a private-duty pediatric nurse, was doing neuro checks every 10 minutes. “I was on top of everything, and it was a double-edged sword,” she says. “It helped reassure me, but having a lot of knowledge also made me more paranoid.”
Fraser and Shah followed Bryan closely in clinic for about a year. During that time, he saw pediatric otolaryngologist Zi Yang Jiang, MD, an associate professor in the Department of Otorhinolaryngology-Head and Neck Surgery at the medical school. Jiang performed a tympanostomy, placing ear tubes for otitis media. He also saw Layla Ghergherehchi, MD, director of the pediatric ophthalmology clinic at the Cizik Eye Clinic and an assistant professor in the Ruiz Department of Ophthalmology and Visual Science at McGovern Medical School. Ghergherehchi monitored his vision and regularly checked pressure on the optic nerves caused by his high ICP.
“An entire team had Bryan under their care at Children’s Memorial Hermann. They treated him as a whole patient and not just as the thrombosis he had,” Blanco says. “At first they saw him every month because he was having headaches and we wanted to rule out seizures. Dr. Fraser ordered an EEG and during that time, Bryan had several CT scans and MRI studies to make sure his intracranial pressure was decreasing. We watched it lower every three months as we checked it. A year later they repeated the pressure measurement and found his pressure had returned to normal.”
Fraser says Blanco did a great job of managing her son’s referrals, allowing the team to provide a high level of care. “She was so on top of things and such a good advocate for him,” he says. “We hoped to avoid surgery and a year later that proved to be the right decision. The watchful waiting we did with the medication was very routine for us. The blood clot on the right solidified and is occluded, but his left transverse sinus, which was not much bigger than the head of a pencil, grew enough that we were able to stop Bryan’s medication.”
Fraser also wrote a letter in support of insurance payment for 40 hours a week of Applied Behavioral Analysis Therapy (ABA), the gold standard for education of children with autism spectrum disorders. Bryan started ABA in August 2021 and completed a year. In August 2022, he enrolled in kindergarten and finished this year.
“He knows how to read, multiply, add, and subtract,” says his mother. “Math is his favorite subject. He’s in a special education program – a regular class but smaller than normal with nine students so that they have more support.” Fraser noted his improvement over a period of six months. “He began to talk much more, could carry on a conversation, and could tell me if he had pain,” the neurologist says. “He remembered my name and always asked what we were going to do during the appointment. He had been through so much because of his ear infection, and he came out the other end a much stronger boy.”
Blanco thanks the entire team. “They were all wonderful for Bryan,” she says. “If we hadn’t changed our route and hospitals, we don’t know where Bryan would be. I’m very grateful to all of them for helping my son. Bryan got the care he needed, when he needed it, and avoided what could have been a major life-altering stroke.”
Inside this Edition:
- Responsive Neurostimulation for Generalized Epilepsy in an 18-Year-Old
- The NICU Follow-Up Clinic: Everything Premature Babies Need To Get the Best Start in Life
- Team-Based Medicine Leads to Nonsurgical Repair of Depressed Skull Fractures in Two Neonates
- Watchful Waiting for Cerebral Venous Thrombosis Allows a Boy To Avoid Brain Surgery
- UTHealth Houston Team Completes Feasibility Study for Minimally Invasive Myelomeningocele Repair in 25 Patients
- Developing Better Laboratory Models of Neonatal Intraventricular Hemorrhage and Hydrocephalus
- Researchers Seek to Improve Outcomes in Children with Malignant Fourth Ventricular Brain Tumors Through Novel Studies
- McGovern Medical School Alumni Blend Neurology Expertise and Philanthropy To Advance Pediatric Tumor Research