Translational Science Program Working to Identify Therapeutic Targets in Chronic Rhinosinusitis
 Otorhinolaryngologists at Memorial Hermann-Texas Medical Center and McGovern Medical School are currently working to identify novel therapeutic targets they hope will lead to the development of more effective therapies for chronic rhinosinusitis (CRS). During the past year, the researchers presented data at meetings of the American Association of Immunologists (AAI), American Association of Allergy, Asthma and Immunology (AAAAI) and a recent Keystone Symposium on Molecular and Cellular Biology.
Otorhinolaryngologists at Memorial Hermann-Texas Medical Center and McGovern Medical School are currently working to identify novel therapeutic targets they hope will lead to the development of more effective therapies for chronic rhinosinusitis (CRS). During the past year, the researchers presented data at meetings of the American Association of Immunologists (AAI), American Association of Allergy, Asthma and Immunology (AAAAI) and a recent Keystone Symposium on Molecular and Cellular Biology.
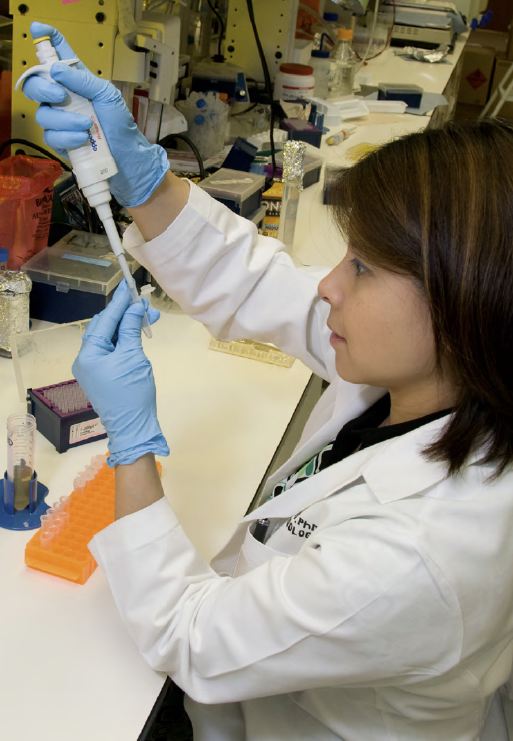 Ongoing research projects include an examination of the role of the newly identified innate lymphoid cell (ILC), which has been shown to produce interleukin 13 (IL-13) in murine models of allergic asthma. “We’ve noted an increased number of these cells in CRS patients with nasal polyps, and they appear to be downstream of an epithelial cell-derived cytokine called interleukin 33 (IL-33), which is released in response to fungal antigens,” says Amber U. Luong, MD, PhD, a physician-scientist who serves as an assistant professor in the department of Otorhinolaryngology—Head and Neck Surgery and directs a lab at the UTHealth/Brown Foundation Institute of Molecular Medicine. “We’re dissecting out the molecular pathway for this new cytokine and studying its association with CRS, as well as looking for other target cells for IL-33. By delving into the pathways initiated by IL-33, we hope to better understand the pathophysiology of CRS and identify novel therapeutic targets that will lead to the development of better therapeutic agents based on the clinical presentation and cause of disease.”
Ongoing research projects include an examination of the role of the newly identified innate lymphoid cell (ILC), which has been shown to produce interleukin 13 (IL-13) in murine models of allergic asthma. “We’ve noted an increased number of these cells in CRS patients with nasal polyps, and they appear to be downstream of an epithelial cell-derived cytokine called interleukin 33 (IL-33), which is released in response to fungal antigens,” says Amber U. Luong, MD, PhD, a physician-scientist who serves as an assistant professor in the department of Otorhinolaryngology—Head and Neck Surgery and directs a lab at the UTHealth/Brown Foundation Institute of Molecular Medicine. “We’re dissecting out the molecular pathway for this new cytokine and studying its association with CRS, as well as looking for other target cells for IL-33. By delving into the pathways initiated by IL-33, we hope to better understand the pathophysiology of CRS and identify novel therapeutic targets that will lead to the development of better therapeutic agents based on the clinical presentation and cause of disease.”
Dr. Luong and her research team are also establishing a database that will include molecular profiles of CRS patients. “CRS has a common clinical presentation and symptoms, but various agents can trigger the condition,” she says. “We can categorize patients by the presence or absence of polyps, or history of atopic status, but we currently do not have an objective means of subtyping these various clinical presentations of CRS. Establishing and categorizing CRS subtypes based on a molecular profile will not only help us understand the origin of the condition but also will be the first necessary step toward personalized medical therapy.”