Newsletter
Quality Quarterly, Pediatric Surgery Quality Collaborative
September 2025

Thanks to all of you who attended our in-person meeting in July at the ACS Quality and Safety Conference. We had a great turnout and continue to be im-pressed by your commitment to improving pediatric surgery.
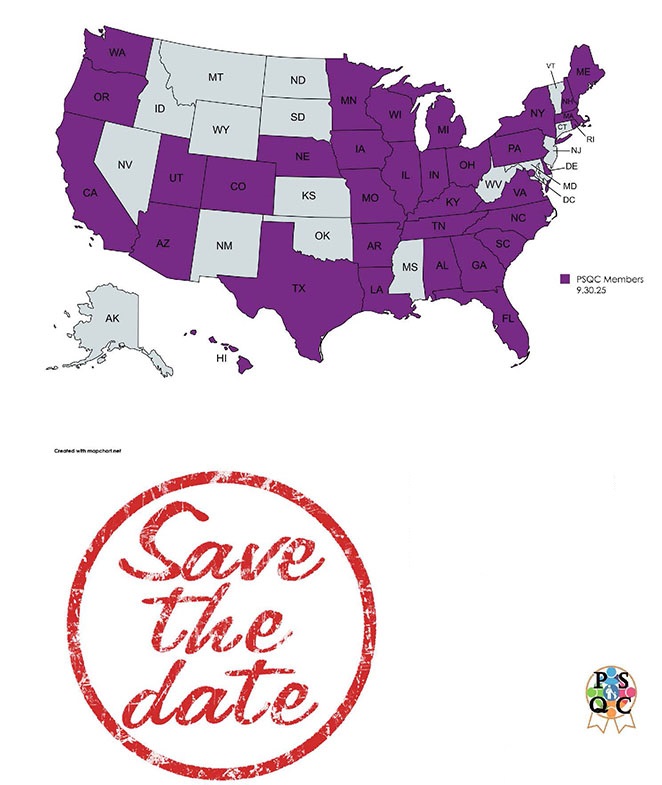
We are continuing our transition to membership in the PSQC being defined as having a data use agreement (DUA) between the University of Texas Health Science Center at Houston and your hospital. The intent of this approach is to pro-vide a broad platform for quality improvement projects now and in the future with which you can participate without needing to execute an agreement for each project. We are currently at 67 sites with an executed DUA. We anticipate that number will increase to around 85 sites.
The ACS Children’s Surgery Clinical Collaborative (CSCC) is moving forward on the opioid reduction project to include ENT, Urology, Plastic Surgery and Orthopedics. If you are not aware or interested, we can provide you with contact information.
We are wrapping up our antibiotic stewardship project and will share our findings with all members around the end of the year. You will find information on our newest project discussion around gastrostomy tubes within.
Thank you for your continued interest in Quality via the PSQC. If you have any questions about anything PSQC or are interested in pursuing a project, please reach out to Terry.
Kevin Lally, MD, MS, FACS PSQC Executive Director
Surgeon-in-Chief, Children’s Memorial Hermann Hospital
Houston, TX

PSQC Projects
Executive Summary of In-Person Meeting
Antibiotic Duration post Appendectomy for Complicated Appendicitis
This project aimed to assess the effect an antibiotic protocol of 4 days (+/- 1) , based on the STOP-IT trial, would have on patients undergoing an appendectomy for complicated appendicitis. Of primary interest was what effect a shortened course might have on rates of SSIs and readmissions. 36 hospitals participated in this project, with 21 adopting the protocol and 15 continuing usual care. Each participating hospital submitted data to PSQC on a quarterly basis.
Our analysis of a cohort of patients between July 1, 2023 and June 30, 2024, demonstrates that patients who receive a shorter course (median 5 days) did not have a higher propensity for SSIs or readmissions. The protocol patients and usual care patients (median 8 days of antibiotics) had no significant difference in their rates of SSIs, readmissions or ED visits. Our research resident, Dr. Jeannette Joly, presented on these findings at the American Surgical Association annual meeting in April. The findings have been published. You can review the abstract here.
Our next steps on this project will be an assessment of best approaches to adoption and how to scale-up the adoption of this protocol across children’s hospitals.
Antibiotic Stewardship
This project was developed using the SAP SAR from 30 participating hospitals as well as a survey of practices from those same hospitals. Using the survey and SAP SAR information, 14 hospitals were identified as good candidates for qualitative interviews.
The interviews focused on how teams make use of the SAP SAR and if the site has been able to effect any changes in their antibiotic utilization using the SAP SAR as well as other methods adopted to reduce antibiotic utilization in the post operative period.
Emerging themes are: Champion is essential; Utilization of antibiotic dosing protocol effective; Feedback on performance supports change; Dissemination of the SAP SAR does influence behavior. A comprehensive document on best practices and tools will be provided to all PSQC members by the end of the year.
G-Tube
With the NSQIP Pilot on gtubes having 73 participating hospitals, the data is now available for robust quality improvement projects. Initial findings from the pilot indicate: wide variability in utilization of upper GI (UGI) series pre-operatively; accidental dislodgement at 0-30 days; and accidental dislodgement at 31-60 days. The evidence suggests that UGIs should not be performed routinely but only when clinically indicated. Accidental dislodgment is a stickier issue as these tend to occur outside hospital control after dis-charge but likely account for a majority of return to systems. We anticipate several pro-jects will develop in this group over the next two years.
Potential project ideas: reduction of accidental dislodgments; reduction of routine use of UGIs and how to reduce returns to system.
Other Presentations from PSQC In-Person Meeting
A panel presentation from SCRs and CSPMs from member hospitals on their various quality improvement projects and strategies for success closed our meeting. Deborah Liebrecht of Colorado Children’s, discussed improving feedback on post-op occurrences through automation and build of a data dashboard. Improved data transparency with surgical teams in a large system increases awareness and ability to develop necessary quality improvement projects. Perioperative Performance Improvement and Patient Safety (PIPS) team can now focus on high-level, system-wide projects while delegating case reviews to surgical division QI leads with options to escalate as needed (PIPS re-view, M&M, root cause analysis). Betsy Diep of Kaiser SoCal, discussed how to partner with your surgeons on improving standardization of practice. Karissa Price of Dallas Children’s shared her hospital’s Development and Implementation of On-Demand NSQIP Visualization Tools in a Pediatric Health System dashboard using Tableau.
The panel presentation was an opportunity for attendees to ask questions and share their own experiences with the assembled panel and all attendees. There were no formal presentations for the panel and thus none are included in the addendum.
PSQC Organization Update
The ACS has formed a QI collaborative called the Children’s Surgery Collaborative (CSC) with its first project focused on opioid stewardship. ACS has begun recruitment of participants and is hosting webinars to discuss the project and how to become involved.
We have contacted all the NSQIP-P hospitals within the U.S. and invited them to join the PSQC. We will be extending the invitation to our inter-national colleagues as well. This DUA will encompass any QI project we’d like to pursue for the foreseeable future with the PSQC evolving into a largely general surgery focused QI collaborative.
The College has not shared data with PSQC since July 2021, so that DUA is essentially nonfunctional as the ACS collaborative won’t need it. The new DUA will be between your hospital and the University of Texas and will define membership in the PSQC. It will be a standing DUA meaning your hospital can opt to participate in any QI project that PSQC launches or not.
There is no requirement to participate. This is completely voluntary. But we do hope you will. We are finding that work done by this collaborative is having a significant impact on care patterns in general surgery.
If you have any questions, please reach out to Terry.
Welcome New Members!
Please contact Terry Fisher to request the full list of our new members!
PSQC In-Person Meeting
Thursday, July 30th
1-5pm EDT
Orlando, FL
 Recent Publications of Interest by Our Members
Recent Publications of Interest by Our Members
The protocol was adopted by 21 hospitals; 15 continued usual care. Across hospitals, 1934 patients were analyzed: 1046 protocol, 888 usual care. The median age was 10 years (IQR: 7.3-13.2), 59% were male. Thirty-day SSI rate was 13% (91% organ space). In multivariable regression, the protocol group had fewer antibiotic days (RR: 0.69, 95% confidence interval [CI]: 0.62-0.78): mean of 5.8 days versus 8.4 for usual care, a difference of 2.6 fewer antibiotic days (95% CI: 1.73-3.37). Multivariable regression showed no difference in 30-day SSI rates between groups (12.7% vs. 13.6%) (OR: 0.96, 95% CI: 0.63-1.47).
Conclusion: This PSQC effort demonstrates widespread standardization of care and quality improvement in pediatric surgery through multicenter adoption of an evidence-based, short-course antibiotic protocol. Protocol adoption was associated with fewer antibiotic days without increasing 30-day SSI.
Tracheostomy Outcomes in Children With Bronchopulmonary Dysplasia
There were 76 patients included in this study. The overall mortality was 30.3% (23/76) with one tracheostomy-related death. Tracheostomy occurred at a median 56 weeks postmenstrual age (PMA). Tracheitis was the most common short- and long-term adverse event (within the first postoperative week, 21%; after postoperative day 7, 81%). Other complications observed include stomal granuloma (77%), airway stenosis (69%), and accidental decannulation (38%). The 30-day and 2-year readmission rates were 32% and 61%, of which 61% and 76% were for tracheostomy-related causes, respectively. The most common reason for readmission over these time periods was tracheitis. Overall decannulation rate for surviving patients was 68%, and decannulation occurred at a median 3.1 years of age. Most surviving patients returned for operative airway intervention (85%); 43% required open airway reconstruction.
We aimed to evaluate the incidence of preoperative anemia and transfusion over the last 11 yr and the association between anemia, transfusion, and postoperative outcomes in children undergoing noncardiac surgery. The incidence of preoperative anemia and transfusion in children have remained stable in the last 11 yr. Anemia, transfusion, and the combination of both in-creased 30-day mortality and the incidence of postoperative complications.
Management of pediatric traumatic lower extremity vascular injuries
Pediatric lower extremity vascular injuries are challenging to manage and treat. Early recognition and a high index of suspicion is needed to ensure accurate diagnosis and timely interventions to prevent limb loss. These injuries present numerous technical challenges to the surgical multidisciplinary team, particularly in a very young patient. Technical challenges relate to small vessel size, vasospasm, and at times the lack of a suitable conduit for vascular reconstructions. The literature describing accepted clinical algorithms and techniques to manage these patients and their injuries are sparse. Moreover, there is significant variability in clinical specialties involved in their care.
Projected Lifetime Cancer Risks From Current Computed Tomography Imaging
An estimated 61 510 000 patients underwent 93 000 000 CT examinations in 2023, including 2 570 000 (4.2%) children, 58 940 000 (95.8%) adults, 32 600 000 (53.0%) female patients, and 28 910 000 (47.0%) male patients. Approximately 103 000 (90% UL, 96 400-109 500) radiation-induced cancers were projected to result from these examinations. Estimated radiation-induced cancer risks were higher in children and adolescents, yet higher CT utilization in adults accounted for most (93 000; 90% UL, 86 900-99 600 [91%]) radiation-induced cancers. The most common cancers were lung cancer (22 400 cases; 90% UL, 20 200-25 000 cases), colon cancer (8700 cases; 90% UL, 7800-9700 cases), leukemia (7900 cas-es; 90% UL, 6700-9500 cases), and bladder cancer (7100 cases, 90% UL, 6000-8500 cases) overall, while in female patients, breast was second most common (5700 cases; 90% UL, 5000-6500 cases). The largest number of cancers was pro-jected to result from abdomen and pelvis CT in adults, reflecting 37 500 of 103 000 cancers (37%) and 30 million of 93 million CT examinations (32%), followed by chest CT (21 500 cancers [21%]; 20 million examinations [21%]). Estimates remained large over a variety of sensitivity analyses, which resulted in a range of 80 000 to 127 000 projected cancers across analyses.
Conclusions and relevance: This study found that at current utilization and radiation dose levels, CT examinations in 2023 were projected to result in approximately 103 000 future cancers over the course of the lifetime of exposed patients. If current practices persist, CT-associated cancer could eventually account for 5% of all new cancer diagnoses annually.

Hello all!
Thanks so much to all the SCRs from pilot hospitals who have been so generous with their time in sending me data reports for the projects. None of this works without you!
The abx duration project is entering its next phase. We are examining best ways to scale up utilization of the PSQC protocol.
GTube project just getting started. Let me know if your hospital wants to participate.
Please email me at [email protected] if you have any questions or I can help in any way.
Terry
Terry Fisher, MPH, PMP
PSQC Program Manager, McGovern Medical School
Houston, TX
*Please contact Terry Fisher to request the full newsletter.
Return to PSQC Homepage