BLOOD AND THE BRAIN: Advancing trauma care through research
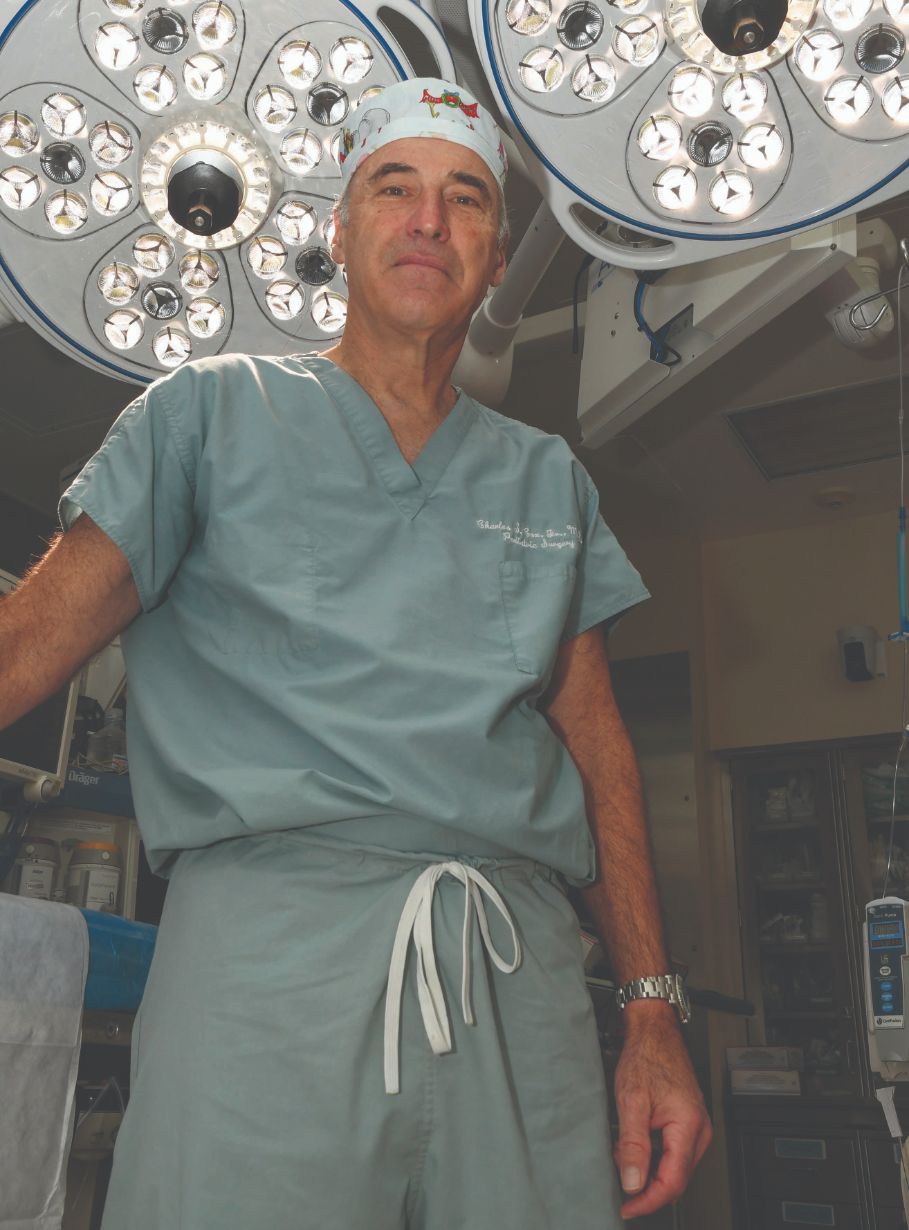
Dr. Charles Cox leads research to understand effects of disruptions in the blood-brain barrier.
Improving patient outcomes by unraveling the intricate mechanisms of hemorrhagic shock and the blood-brain barrier are goals of two new research grants received by IMM faculty member Charles Cox, MD.
The blood-brain barrier, a crucial component in maintaining brain function, regulates the passage of substances from the blood to the brain. Cox’s research is dedicated to understanding how disruptions in this barrier contribute to brain injury and hemorrhagic shock, two factors that significantly impact patient outcomes.
“If you get run over by a bus today, you’re most likely going to bleed to death, or have the consequences of hemorrhagic shock,” said Cox, the George and Cynthia Mitchell Distinguished Chair in Neurosciences and a Bentsen Stroke Center Investigator at the IMM. “The reason we study those two, and the interplay between them, is because that’s why you die after you’re injured.”
Trauma is the leading cause of death for those up to 45 years old and the fourth-leading cause of death for all ages in the United States. Traumatic brain injury is the single largest cause of death from injury in the United States, and 60,000 die yearly from excessive blood loss.
Armed with two four-year program focus awards totaling nearly $9 million from the Department of Defense, Cox and his lab are seeking to curb these statistics.
“Trauma studies in the civilian population have direct correlates to military injuries and vice-versa,” explained Cox, the Glassell Family Distinguished Chair in Pediatric Surgery, and director of the Pediatric Surgical Translational Laboratories and Pediatric Program in Regenerative Medicine. “The reason we can do this research and clinical trials is because of the high level of trauma patients we see at Memorial Hermann-Texas Medical Center.”
Understanding how trauma, bleeding, and resuscitation impact the brain is essential for developing effective treatment strategies. This work addresses real-world issues, including the dysregulated coagulation that follows brain injury, leading to increased bleeding and compromised clotting mechanisms.
“We are trying to understand how the brain responds to this resuscitation and how it is impacted,” he said.
A newly designed 3D cell model of the blood brain barrier helps the team measure processes at a cellular level and recapitulate the physiology of the blood brain barrier.
“Our model mimics the neurovascular unit within your brain and is foundational for our work,” he said.
In addition to the lab work, Cox’s team is actively engaged in clinical trials, including a phase two trial on stemcell-based therapeutics for chronic brain injury. They also lead a multi-center clinical trial exploring whole blood and adjunct to whole blood resuscitation for severe injuries in children.
As the research progresses, the potential for mitigating the consequences of severe injuries becomes increasingly tangible.
Cox and his team are not just uncovering the mysteries of hemorrhagic shock and the blood-brain barrier— they are paving the way for transformative treatments.
