UTHealth Houston joins SATURN trial
A clinical trial evaluating the role of statins in the risk of recurrent intracerebral hemorrhage (ICH) in patients presenting with ICH, has opened for enrollment at UTHealth Houston.
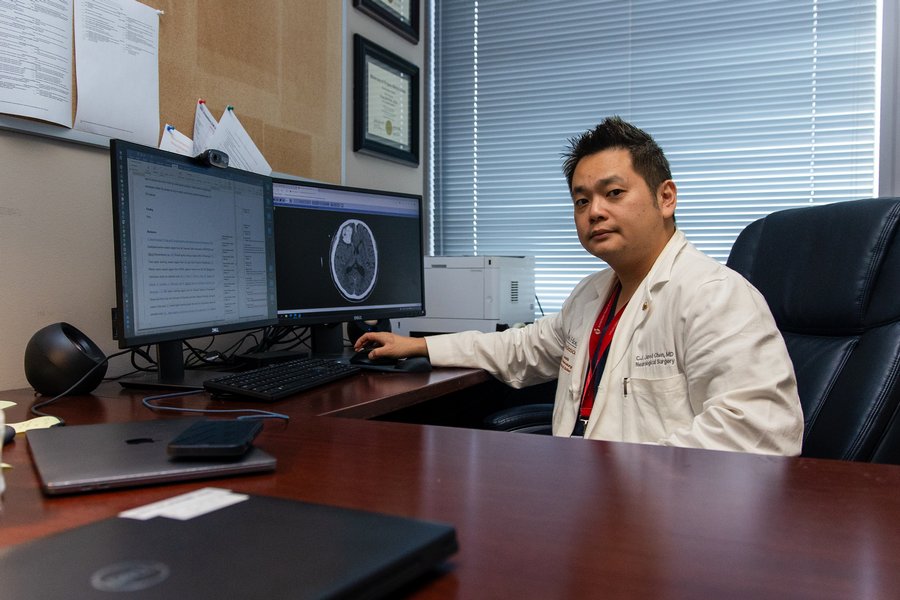
The study, led locally by C.J. Jared Chen, MD, assistant professor in the Vivian L. Smith Department of Neurosurgery, will enroll patients at Memorial Hermann-Texas Medical Center and Memorial Hermann-Memorial City. The sites are among the planned 140 to join the SATURN trial, which is being funded by the National Institutes of Health National Institute of Neurological Disorders and Stroke (NIH/NINDS) and coordinated through the NIH/NINDS StrokeNet and the Canadian Stroke Consortium.
ICH, which is a form of hemorrhagic stroke, occurs when a small blood vessel ruptures and causes bleeding into the brain. It is the second-most common cause of stroke, accounting for some 15% to 30% of strokes, and the deadliest. Because of this, it requires emergency care, usually involving medications and close monitoring in an intensive care unit.
Statins are widely prescribed for primary and secondary prevention of ischemic cardiac and cerebrovascular diseases. However, previous research has suggested that statins increase ICH risk in people with a history of hemorrhagic stroke, which has led to uncertainty regarding the risks versus benefits of statin therapy for former stroke patients.
“For ICH patients who are on statins, there may be a higher risk of recurrent ICH because of statins’ association with cerebral microbleeds and its potential antithrombotic effects. On the contrary, without statins, these patients may be at risk for ischemic cardio/cerebrovascular events,” Chen said. “It’s weighing the risk of recurrent ICH versus the risk of these ischemic events, but ultimately, which of these is better for these patients? Do we continue the statin, or stop it? That’s what the study will answer.”
In total, SATURN — a multicenter, pragmatic, prospective, randomized, open-label, and blinded end-point assessment clinical trial — expects to enroll 1,456 patients presenting within seven days of a spontaneous lobar ICH while taking statins. Spontaneous lobar ICH is a nontraumatic form of ICH, where the brain bleed occurs in one of the central lobes.
Patients will be randomized to one of two treatment groups: discontinuation versus continuation of statin therapy. Participants will be followed for a two-year period to track the occurrence of recurrent symptomatic ICH or major adverse cerebrovascular or cardiovascular events during the follow-up period.
A subset of patients will also participate in the optional magnetic resonance imaging (MRI) ancillary study, where they will undergo a baseline MRI within seven days of randomization into the study, and a repeat MRI at the end of the follow-up period.
“The MRI ancillary study will provide us with more insight into the association between statins and cerebral microbleeds,” Chen said. “The incidence of new cerebral microbleeds will be compared between patients who continued statins and those who stopped statins in the ancillary study.”
Chen aims to recruit 50 patients at the Memorial Hermann-TMC and Memorial Hermann-Memorial City sites. Participants must be at least 50 years old, with a spontaneous lobar ICH confirmed by a computed tomography (CT) or MRI scan within the past seven days, and had to have been taking a statin drug at the onset of the ICH, among other qualifications.
For more information on the SATURN trial, visit clinicaltrials.gov.