Laboratory of H. Alex Choi, M.D.
OVERVIEW
H. Alex Choi, M.D. is an Assistant Professor and neurointensivist at McGovern Medical School at UTHealth. His work focuses on research that improves patient outcomes after acute brain injury, particularly aneurysmal Subarachnoid Hemorrhage (SAH). He is interested in employing statistical, informatics and machine learning approaches to addresses some critical problems in the Neuroscience Intensive Care Unit (NICU). Major research interests focus on (a) prediction of secondary complications such as delayed cerebral ischemia (DCI) after SAH (b) understanding abnormal neuroinflammatory activity after acute brain injury and their association with poor outcomes. Currently, the lab is focused on using network informatics approaches to model and analyze the immune profile. The immune response is complex and dynamic involving hundreds of interactions and cells and molecules. Conventional statistical methods fail to account for this intricacy. The novel bioinformatics tools developed will seek to unravel this complexity and provide deeper insights into the nature of the immune profile and (c) Clinical research/trials pertaining to SAH; working in concert with labs (Dr.Pramod Dash) involved in preclinical research to test novel anti-inflammatory therapeutics after acute brain injury.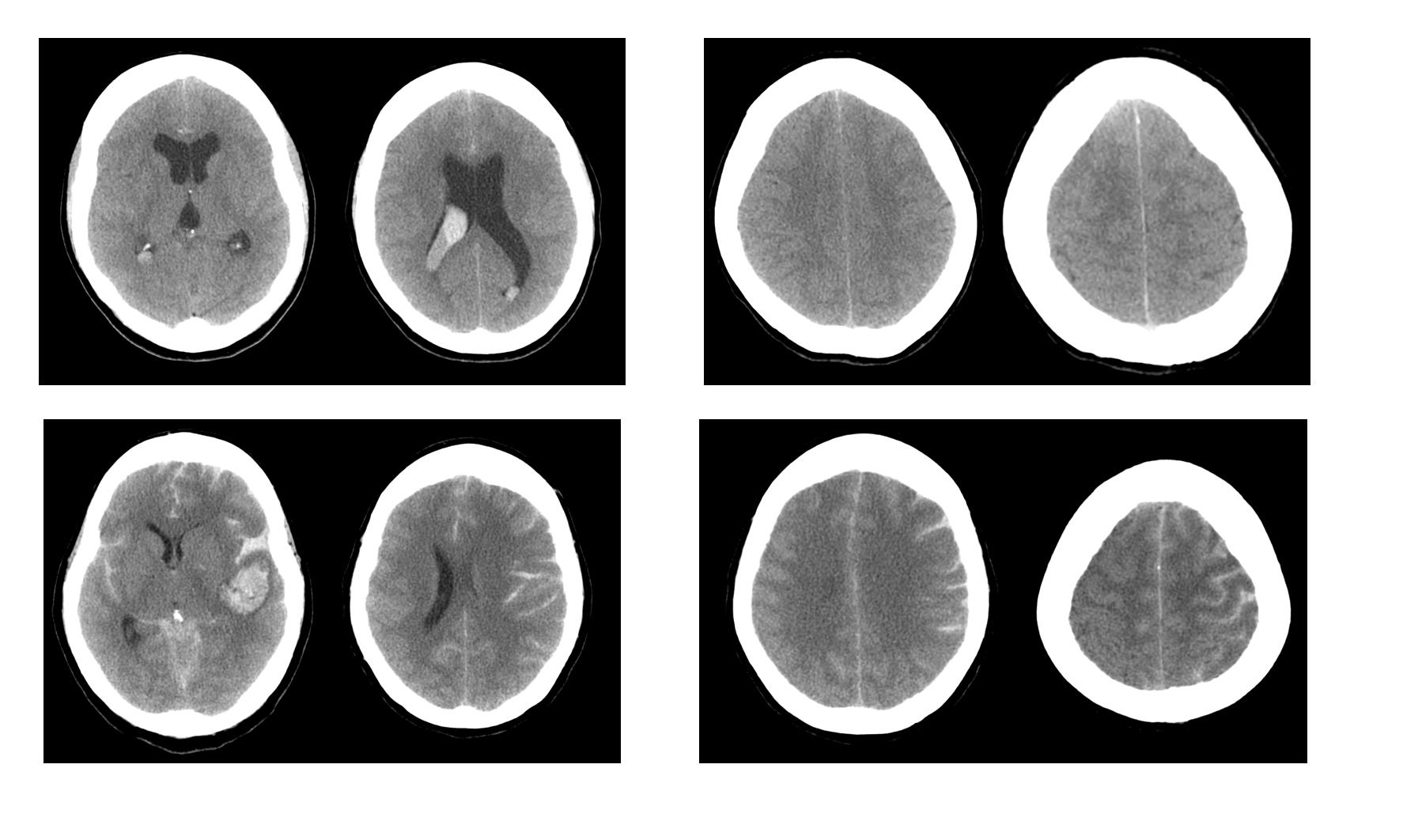
CURRENT PROJECTS
1) Machine Learning techniques for prediction of secondary complications after SAH
Some SAH patients in the ICU are at increased risk of developing dangerous secondary complications such as delayed cerebral ischemia (DCI). In patients with DCI, there is a sudden loss of blood flow to vital brain regions that can result in severe morbidity or mortality. If these at-risk patients are identified early on, a physician can prophylactically treat and monitor them diligently to mitigate symptoms. Currently, there are no effective methods to asses a patient’s risk of developing DCI. We will develop novel machine learning algorithms that can predict whether or not a patient will develop DCI by utilizing easily available data such as lab reports, vital signs and admission status.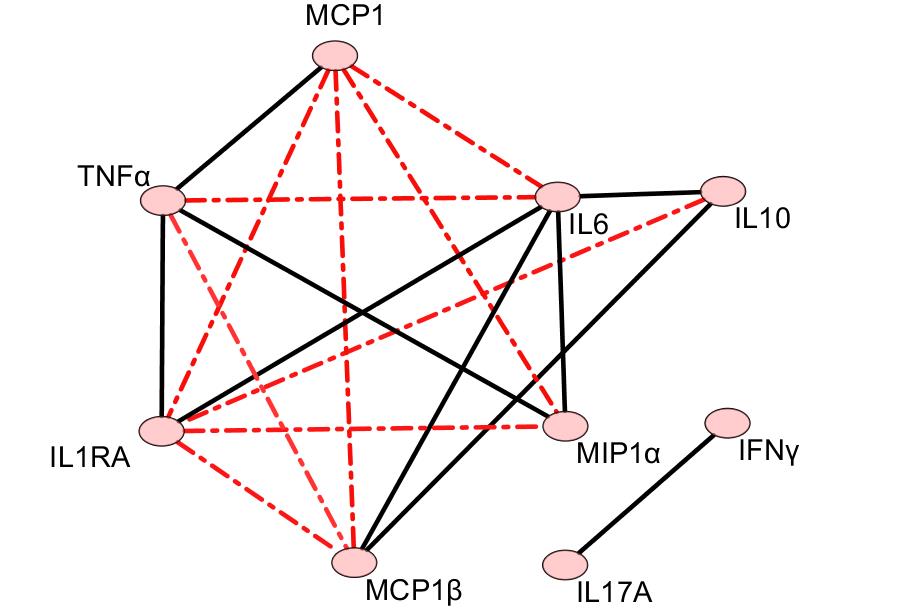
2) Inflammatory cytokine pathways after SAH
Uncontrolled neuroinflammation after acute brain injury is a significant contributor to secondary brain injury and poor outcomes. We will first experimentally determine inflammatory cytokine levels in serum and CSF collected from SAH patients at the NICU. Using novel bioinformatics clustering and network analysis tools, we will discover pathways within the inflammatory profile that favors poor outcomes and good patient outcomes.
3) Cerebral Edema
Cerebral Edema (CE) after SAH is associated with poor outcomes. The pathomechanism of GCE is unclear. GCE may represent vulnerable tissue status to microcirculatory ischemia. Patients with CE are at risk of developing DCI and vasospasms. We will develop a novel cerebral edema scoring system based on admission status with the idea of building a predictive system for DCI and vasospasm.
4) Thromboelastographic correlation with neurological complications and outcome in subarachnoid hemorrhage patients
Thromboelastography (TEG) is the broadly applied for detecting coagulation, platelet function, and fibrinolysis abnormality of various clinical situations recently. In several studies on intracranial hemorrhage, ischemic stroke, and traumatic brain injury reported, TEG shows correlation with severity of the disease and complications. In subarachnoid hemorrhage (SAH) patients, long-term outcome and mortality were determined by complications such as re-bleeding and delayed cerebral ischemia.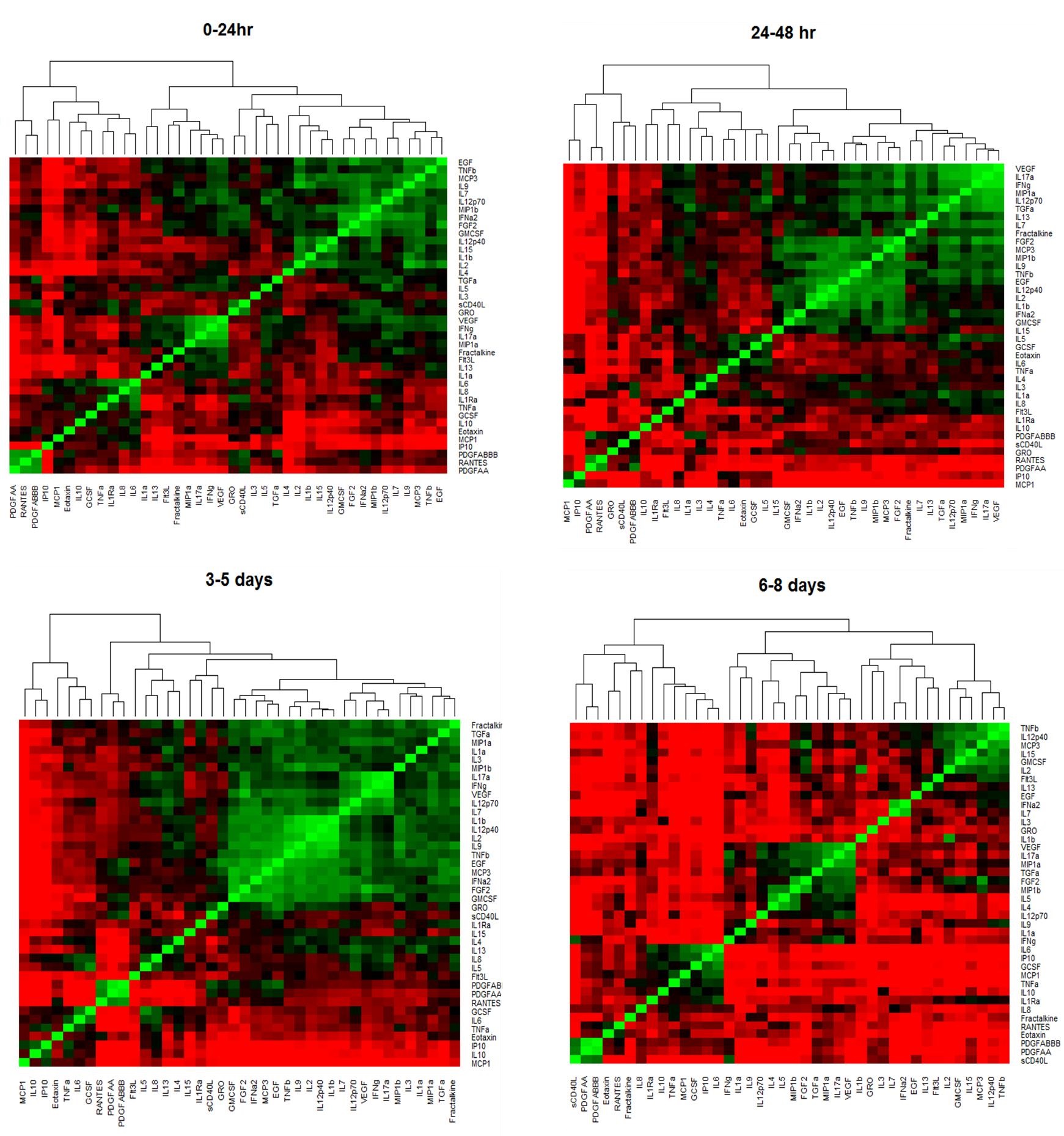 We investigate TEG as a tool in SAH patients to find association with complications and outcome.
We investigate TEG as a tool in SAH patients to find association with complications and outcome.
5) Pharmaceutical studies Steroid and Statins
This study is focused on determining if administration of steroids and statins improve outcomes.
6) Venous Thromboembolism and Complications in Hospitalized Patients
This study is focused on comprehensive analysis of the epidemiologic features including incidence, complications associated with prophylaxis or management, and outcome in hospitalized patients with venous thromboembolism (VTE). VTE is induced by stasis of venous blood particularly in hypercoagulative condition, such as old age, active cancer, and neurological disease with limb paresis, major surgery, and trauma. VTE is common disease in hospitalized patients and associated with reduced survival and increased morbidity. Therefore, understanding about VTE in various hospitalized patients might be helpful for proper prevention of VTE and improvement of overall outcome. In this study, we analyze the data of hospitalized patients retrospectively to find the clinical implications of VTE incidence, complications, and outcome for adequate prevention and management of VTE.
7) Quantification of Vasospasm
Cerebral vasospasm is well-known sequelae of aneurysmal SAH. We developing novel imaging biomarkers for quantification of early vasospasm and testing its predictive ability to predict DCI after SAH.
TEAM MEMBERS
H Alex Choi, M.D. Assistant Professor and Principal Investigator
Jude Savarraj, Ph.D. Bioinformatics Postdoctoral Fellow
Sungho Ahn, M.D. Visiting Fellow
Jin Park, M.D Visiting Fellow
Wes Jones, M.D Neurosurgery Resident
Mubashir Pervez, M.D Neurology Resident
Elena Espino, B.S. Research Assistant
Sophie Samuel D. Pharm Pharmacy Research
Glenda Torres B.S Research Coordinator
CONTACT
Email: [email protected]
Office Phone: 713.500.6128
RECENT PUBLICATIONS
-
- Choi HA, Ko SB, Chen H, Gilmore E, Carpenter AM, Lee D, Claassen J, Mayer SA, Schmidt JM, Lee K, Connelly ES, Paik M, Badjitia N. Acute effects of nimodipine on cerebral vasculature and brain metabolism in high grade subarachnoid hemorrhage patients. Neurocrit Care. 2012 Jun;16(3):363-7. PMID; 22262041
- Ko SB, Choi HA, Parikh G, Schmidt JM, Lee K, Badjatia N, Claassen J, Connolly ES, Mayer SA. Real time estimation of brain water content in comatose patients. Ann Neurol. 2012 Sep;72(3):344-50. PMCID: PMC3464349
- Ko SB, Choi HA, Parikh G, Helbok R, Schmidt JM, Lee K, Badjatia N, Claassen J, Connolly ES, Mayer SA. Multimodality Monitoring in Comatose Patients with Intracerebral Hemorrhage. Stroke. 2011 Nov;42(11):3087-92.
- Choi HA, Ko SB, Presciutti M, Fernandez L. Carpenter AM, Lesch C, Gilmore E, Malhotra R, Mayer SA, Lee K, Claassen J, Schmidt JM, Badjatia N. Prevention of shivering during therapeutic temperature modulation: The columbia anti-shivering protocol. Neurocritical Care. 14(3): 389-94, June 2011.
- Choi HA, Badjatia N, Mayer SA. Hypothermia for acute brain injury–mechanisms and practical aspects. Nat Rev Neurol. 2012 Feb 28;8(4):214-22. PMID: 22371279
- Hong JM, Lee JS, Song HJ, Jeong HS, Choi HA, Lee K. Therapeutic hypothermia after recanalization in patients with acute ischemic stroke. Stroke. 45(1):134-40, January 2014.