Clinical Rotations
Curriculum
During the inpatient rotations at Memorial Hermann Hospital – Texas Medical Center (MHH), we have primary services for Stroke, General Neurology, Epilepsy Monitoring Unit, and Neuro-Trauma ICU. In addition to these services, residents manage a neurology consult service. Within the Harris Health system, residents run a neurology consult service at Lyndon B. Johnson General Hospital (LBJ). Outpatient clinics include UT Physicians (UTPB) and Smith Clinic.
Stroke
At MHH, there are two primary stroke services. Junior residents rotate on Stroke A with a vascular fellow, while senior residents independently manage patients on Stroke B. Being one of the busiest stroke centers in the country, residents gain hands-on experience evaluating and managing patients of all ages with ischemic stroke, hemorrhagic stroke, and complex cerebrovascular disorders.
Inpatient General Neurology
MHH houses a primary neurology service, which serves the community as a tertiary referral center. The team is comprised of a PGY4 “pre-attending” role, a PGY-2 “senior” role, and two interns. The residents manage patients with pathologies ranging from status epilepticus, myasthenic crisis, Guillain-Barre, multiple sclerosis exacerbations, autoimmune encephalitis, and more.
General Neurology Consults (MHH)
As one of the largest hospitals within the Texas Medical Center, which includes one of the world’s leading cardiovascular units and one of the busiest level I trauma centers, residents are exposed to a wide array of acute neurological conditions with consults from many other primary services. Our consult team includes a consult senior (adult neurology PGY3 or PGY4) and three junior residents (off-service rotators, pediatric neurology residents, adult neurology PGY2s, and neurology interns).
Code Stroke Resident (MHH)
Junior residents receive early exposure evaluating and managing acute stroke care under the supervision of a vascular neurology fellow. Residents become comfortable identifying acute imaging findings, administering TNK, and managing post-TNK care
Neurology Night Float (MHH)
There are two residents on each night, typically a senior and junior role at the beginning of the year. Hours are 5PM – 7AM with a 4-nights on, 2-nights off schedule. Interns will work in the second half of the year with a PGY4 “buddy” guiding them on how to work efficiently and safely on nights. Our night float system is designed to give residents confidence in practicing all fields of inpatient neurology with the support of an additional resident, stroke fellow, and attending.
Neurocritical Care
Residents work in the state of the art 32-bed open-unit NeuroICU with one of the busiest neuro-trauma centers in the region. There are two primary teams within the ICU led by neurointensivists. One team manages primary neurological conditions, such as severe strokes, status epilepticus, and neuromuscular diseases. The second team focuses on patients with neuro-trauma, spine pathologies, and post-operative neurosurgical patients. Residents will rotate on both services during their PGY2 and PGY3 years.
Epilepsy Monitoring Unit
Patients are admitted to the EMU for characterization of events and surgical planning. Emphasis is placed on reviewing continuous EEG recordings with the attending, adjustment of antiseizure medications during the stay, and eventually planning for epilepsy care after discharge. Junior residents will focus on seizure semiology and localization, while learning to read EEGs using the developed curriculum.
LBJ Consults
As part of the Harris Health system, residents gain exposure to a diverse patient population within the county, providing care for the underserved community. Senior residents have the opportunity to truly act in the capacity of an independent consultant while training our internal medicine colleagues in neurologic diseases.
Continuity Clinic
Residents begin continuity clinic as a PGY1 at the Harris Health Outpatient Center, Smith Clinic. Each resident will have a half-day clinic each week except for on night float. During PGY3 year, half of the senior residents will transition to UT Physicians to complete their remaining 2 years of continuity clinic.
Subspecialty Clinics (UTPB and Smith Clinic)
This rotation gives residents the opportunity to experience the different neurological subspecialties. Residents work one-on-one with the attendings in caring for the wide array of patients that come from Houston, other parts of Texas, the Gulf region, or even other parts of the country and the world.
Epilepsy/EEG Course
This is an 8-week course dedicated to developing fellow-level EEG reading skills and to learning about seizure semiology, surgical epilepsy and neuromodulation. All residents have the ability to participate in this course prior to graduation, either as a PGY-2 or PGY-4.
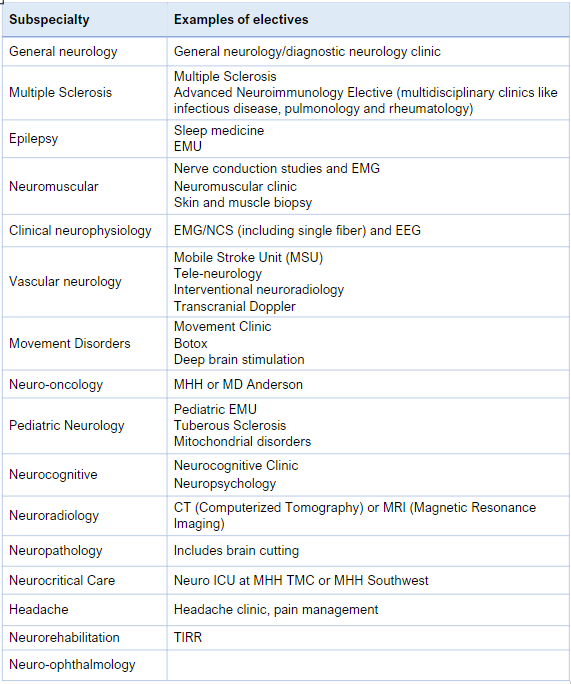
Electives (not comprehensive)