IBD Group 2022 Updates
News Updates: Research on Intestinal Inflammation in the Center for Perioperative Medicine and the Department of Anesthesiology at the McGovern Medical School in Houston
Inflammatory Bowel Disease Research Group: From left, back row: Dr. Xiangsheng Huang, Dr. Agnieszka Czopik, Frank Chen, Dr. Holger Eltzschig. Front row: Victoria Mota, Dr. Xiaoyi Yuan, Dr. Jenifer Baily, Dr. Yanyu Wang.
We would like to express our deep gratitude for the continuing generosity of Mr. Brad McWilliams who has supported our efforts to pursue translational studies to identify new treatment approaches for patients suffering from intestinal inflammation and inflammatory bowel disease (IBD). With the help and support of Brad, we were able to move forward with identifying novel therapeutic targets for IBD that could be game changing for IBD patients. We anticipate that our studies lay the groundwork for clinical trials on hypoxia signaling and miRNAs to prevent or treat excessive intestinal inflammation. These targets would be more specific and most likely have less unwanted side effects as compared to the use of steroids.
Over the past 2 years we have further enhanced and grown our IBD research team to explore novel avenues for therapeutic interventions. Specifically, we found important roles for hypoxia-inducible miRNAs as novel IBD treatment targets. These molecules are powerful regulators in a wide variety of diseases and their roles in IBD has only recently gained appreciation. The small size and portability of miRNAs make them attractive candidates for therapeutic interventions in clinical settings. We envision that miRNA therapies have the potential to become a major class of new drugs to treat bowel inflammation in the coming years.
2021 was a highly successful year filled with new discoveries and research directions. As we begin 2022, we have several exciting updates to share:
Our IBD group has grown.
We recently added the talented and experienced IBD researcher, Dr. Xiangsheng Huang, who joined our team in January 2022. Dr. Huang received his PhD in Biology at the University of Tübingen, Germany. Afterwards, he pursued his postdoctoral training at UTMB and Baylor College of Medicine where he investigated intestinal immune responses to gut microbiota and metabolites in the pathogenesis of IBD. Prior to joining UTHealth, Dr. Huang was an Assistant Researcher at UC Berkeley, where he identified a distinctive role for nuclear receptors in immune regulation of IBD. Through this work, he established in vitro immune cell differentiation techniques and unique murine models of IBD. In addition, Dr. Huang has broad expertise in the role of the purinergic system in modulating intestinal immune responses and has been researching immune cells reactive to commensal bacterial and gut metabolites. His experience, coupled with the Eltzschig Lab expertise in hypoxia-driven pathways, will enable him to establish novel biological paradigms that may lead to future treatment of human inflammatory bowel diseases.
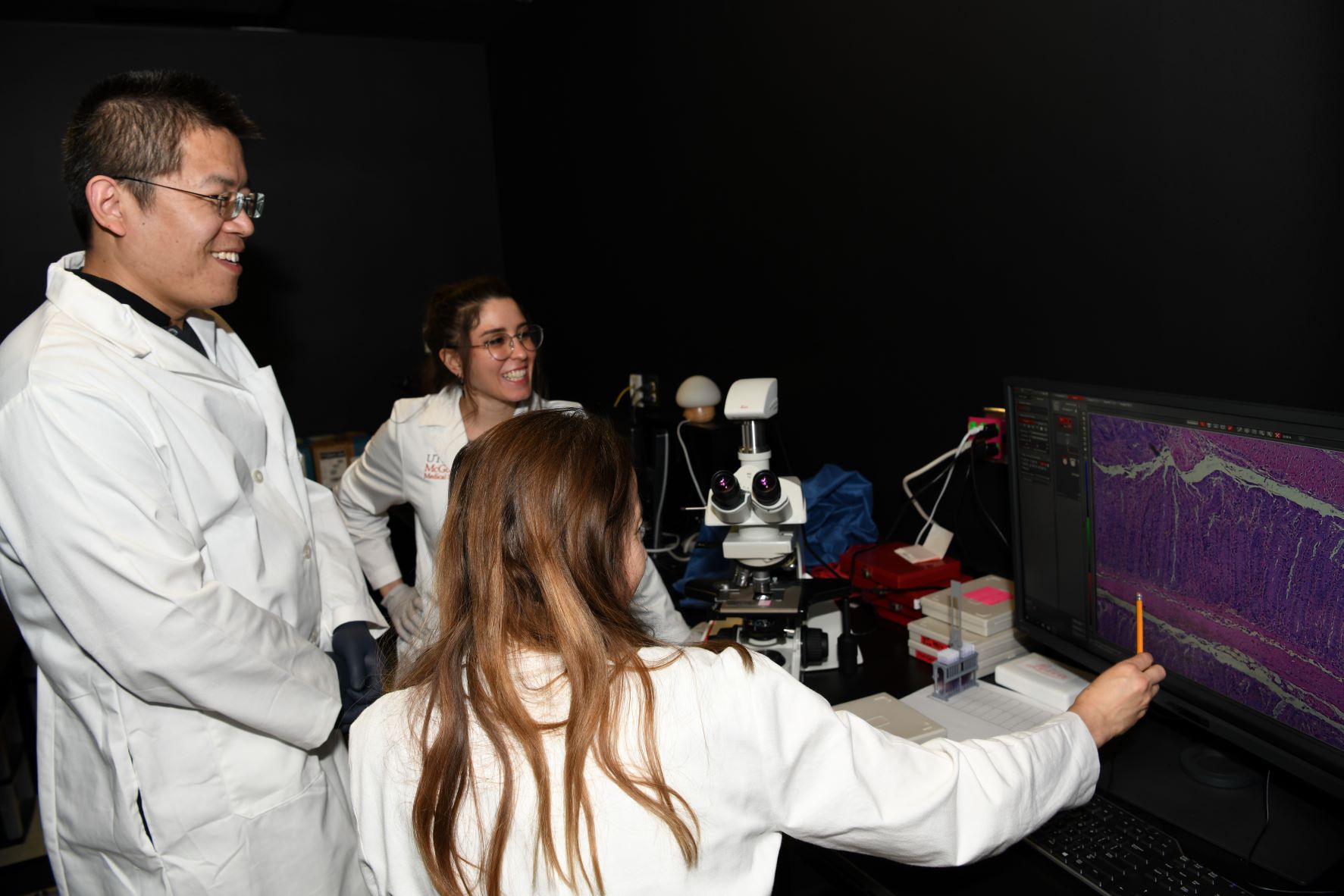
IBD Researchers X. Huang, V. Mota and A. Czopik are studying pathological changes to the bowel in a mouse model of chronic colitis
Victoria Mota, Research Assistant, joined our IBD research group in the summer of 2021. Victoria earned a Bachelor of Science degree in biology from Houston Baptist University in 2021. She has a strong interest in understanding the dynamics of mucosal immunity during IBD and the transgenic murine models utilized for studying colitis. Victoria is eager to broaden her knowledge and increase her technical expertise in molecular biology, immunology, and histology as she helps carry out the daily experimental work. She ultimately plans to apply to graduate programs in molecular biology and immunology, and hopes to become an independent researcher in the future. We are excited to have her in our group and are grateful for her enthusiasm, hard work, and strong drive toward research excellence.
Research Updated from our IBD Program:
Immediate: We have set up colitis models in mice, developed new mutant mouse strains, and designed assays to evaluate the role of the hypoxia/adenosine pathway and microRNAs as regulators of intestinal homeostasis, immune responses, and therapeutic agents in IBD. Our manuscript detailing the role of miR-29, a hypoxia-regulated microRNA, in the development of inflammatory bowel disease and its potential as a therapeutic agent in the clinic is nearing completion. We hope to see this work published in the coming months. The next goal in our studies of miR-29 is to investigate whether this molecule can have a protective effect in the development of colon cancer—a complication which frequently can affect patients who are suffering from IBD over extended time periods.
We have also begun investigation of a second hypoxia-inducible microRNA called miR-147. This molecule has potential anti-inflammatory activity in different cell types. We are studying how miR-147 regulates the function of intestinal lining and the lymphocytes in the layers below the lining. Our preliminary data in mouse models show that miR-147 is essential to maintaining the integrity of the intestine during colitis. We have also found that it may inhibit the overactive lymphocytes in a model of chronic colitis. Our next goal is to verify our findings in human IBD samples and to investigate the mechanisms behind the action of miR-147.
Future Directions:
The new support from Brad McWilliams in conjunction with recently obtained research grants have allowed our group to continue growing and accumulating research data. Based on the novel miR-147 data generated in the past year, we plan to submit a competitive NIH R01 grant application to secure additional resources for the expansion of our investigation into the potential of microRNA-based therapeutics for inflammatory bowel disorders and intestinal cancers. The IBD group generated several novel mouse models and conducted gene-expression screens that will become the cornerstone of our research work and grant-writing efforts in the next few years. We are thankful for the continuing support of Mr. McWilliams and are looking forward to sharing more research highlights this year.
Translating our Findings from Bench to the Bedside: Extensive evidence from ongoing clinical trials with anti-cancer micro RNAs strongly indicates that therapeutic delivery of specific microRNAs may become a robust strategy for IBD therapy as well. Specifically, with optimization of miRNA delivery systems and improvements in the stability of miRNAs the miR-29-mimic, and possibly the miR-147-mimic may soon become a target of a clinical trial aimed to rein in the overactive lymphocytes that promote intestinal inflammation. There are also already-approved therapeutics that activate HIF and induce hypoxia-dependent microRNAs that will be subject of upcoming clinical efforts for successful translation of such therapeutics from bench to bedside. Our pre-clinical data makes a compelling argument for the use of HIF-stabilizing drugs to alleviate suffering of the IBD patients. We will actively pursue in clinical proof-of-principle studies to translate our findings from bench to bedside, and will soon be moving our basic research findings towards clinical trials in patients suffering from excessive inflammation.
We want to close by again thanking Brad McWilliams for the extremely generous support of our IBD research, and his guidance by emphasizing our efforts on bringing the laboratory research findings towards treatments of patients who are suffering from this incredibly devastating disease.