New Study Finds Higher Risk of Complications in Surgical Patients with Cannabis Use Disorder
New Study Finds Higher Risk of Complications in Surgical Patients with Cannabis Use Disorder
A new research study published in JAMA Surgery, the highest-ranking surgical journal in the world, has found that surgical patients with cannabis use disorder have a 20% higher risk of complications during their hospitalization than those without the disorder. Clinical researchers from the Department of Anesthesiology, Critical Care and Pain Medicine at the McGovern Medical School at UTHealth Houston conducted a large nationwide study examining 62,110 major elective surgeries in the United States from 2016-2019. The specific complications analyzed included a combination of myocardial ischemia, acute kidney injury, stroke, respiratory failure, venous thromboembolism, hospital-acquired infection, and surgical procedure-related complication. The findings of this retrospective observational study suggest that cannabis use may pose significant risks to surgical patients.
The number of people using cannabis in the US is increasing because it is becoming more widely legalized and is perceived as harmless. Around 1 in 5 Americans report recent cannabis use, with almost a third of those users developing cannabis use disorder, meaning they continue cannabis use despite the harmful consequences it can have on their physical and mental health. Due to the increase in surgical patients who use cannabis, the American Society of Regional Anesthesia and Pain Medicine has issued new guidelines for the care of these patients. The guidelines recommend that clinicians screen all patients undergoing surgery requiring anesthesia for cannabis use. Previous studies have shown that regular cannabis use can worsen pain and nausea after surgery and increase the need for opioids.
This new study adds to the growing evidence suggesting that cannabis use may negatively affect surgical patients. As rates of cannabis use continue to rise, patients and healthcare providers need to be aware of these potential risks.
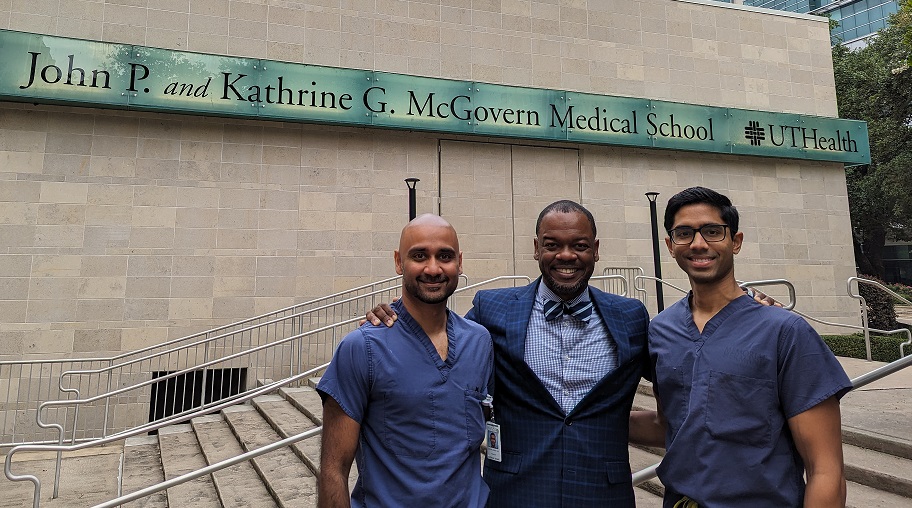
The authors of this study from the Department of Anesthesiology, Critical Care, and Pain Medicine at the McGovern Medical School were Paul Potnuru, MD, Assistant Professor, Director of Airway Education; Srikar Jonna, MD, Assistant Professor, Director of Anesthesiology Critical Care Medicine Fellowship Program; and George W. Williams, II, MD, Professor, Vice Chair, and Division Chief of Critical Care Medicine.
This study was supported by a departmental Research Time Award. You can find the full study here.