Inside Our Fellow’s Daily Routine
Pediatric Operating Rooms
A typical day starts the night before with a conversation with the attending I’m working with. Most of the time this is a text to run through the list and the general plan, though for more complex cases or cases with challenging anatomy, this often becomes a phone call, which is usually a sign that things will be interesting!
On the morning of surgery, I’m up around 5:30 a.m. and at the hospital by about 6:00 a.m. I either see the child and family in pre-op holding to pre-assess and obtain consent, or review the patient on the floor if they are already an inpatient.
The anesthesia technicians are fabulous and make a big difference to how smoothly the day runs. After a quick call or message, they bring and set up anything that’s needed, such as ultrasound, arterial line equipment, or video laryngoscopy. From there, I log into the chart, review the case, draw up medications and prepare the airway equipment.
Once the room is set up, there’s usually time for a quick coffee and to say hello to the attending and others in the department before the first case. Patients are typically in the room by 7:30 a.m., and cases start shortly after.
Once the case is underway and the patient is stable, the attending will offer a morning break. Fellows are guaranteed at least one morning break and a lunch break each day, and because we’re often working one-to-one with attendings, additional breaks are frequently possible. This setup also allows plenty of time for intraoperative teaching and discussion.
For the rest of the day, the attending and I work through the cases assigned to our operating room. Finish times vary depending on the list, but on a regular day I’m usually done before 3:00 p.m., unless I’m pre-call, in which case I’m typically relieved earlier.
This describes a standard non-call day. On-call shifts run from 3:00 p.m. to 7:00 a.m. and are structured quite differently, with responsibility for urgent and emergency cases overnight. I appreciate that fellows typically take only one to two weekday call shifts per week, with no weekend or holiday call.
I also value how well protected our academic time is and how clearly the program prioritizes training over operating room workforce needs.
Before heading home, I usually review the next day’s cases and touch base with the attending to confirm plans.
My decision to pursue pediatric anesthesia fellowship at UT Houston has been one of the most rewarding choices of my career, and I am extremely grateful to have been part of this outstanding, hidden-gem training program.
Pediatric Cardiovascular Anesthesiology
One of the first things you notice on this rotation is how welcoming and supportive everyone is. From the Pedi CV attendings and anesthesiologist assistants who help you with the initial setup, to the operating room staff and surgeons, the entire team is genuinely friendly and helpful.
The day before the procedure, I review the available patient documentation, go over the test results, and present my anesthesia plan to the attending physician I will be working with the next day.
On the day of the procedure, the setup usually takes about 45 minutes. To have the operating room ready by 7:00 AM, I start no later than around 6:15. This gives me enough time to see the patient in pre-op around 7:00 and administer premedication.
In addition to the standard set of medications, I prepare emergency drugs in various dilutions, calcium gluconate, heparin, and tranexamic acid both as a bolus and in an infusion pump. I also prepare a dose of tranexamic acid for the perfusion team to administer into the CPB pump.
The setup typically includes preparing five infusion pumps with: epinephrine, milrinone, and D5NS as a carrier running through the central line, along with pumps for precedex and tranexamic acid connected to a peripheral IV.
Every patient scheduled for CPB case is typically set up with two peripheral IV, a central venous catheter, and an arterial line. Performing these procedures daily provides an excellent opportunity to refine and significantly improve your technical skills.
In addition to cases involving CPB, I also have the opportunity to provide anesthesia in the cardiac catheterization lab and the electrophysiology (EP) lab.
During this rotation, I have had an excellent chance to review and solidify my knowledge of various congenital heart defects and their anesthetic implications, including the management of single-ventricle physiology, pulmonary hypertension, and hemodynamically complex patients.
Pediatric Intensive Care Unit:
My day in the Pediatric ICU typically starts around 7:00 a.m. with morning rounds. Rounds are comprehensive and usually run until early afternoon, offering an in-depth look at a diverse and high-acuity patient population that ranges from neonates to teenagers. At any given time, there are often several patients on ECMO, which makes this an especially rich learning environment.
One of the best aspects of this rotation is its flexibility. There is no firm expectation for fellows to carry patients, but participation is very much tailored to individual interests. If you have a strong interest in pediatric critical care, you are encouraged to be as involved as you’d like by taking ownership of patients, engaging in clinical decision-making, and participating in complex care discussions.
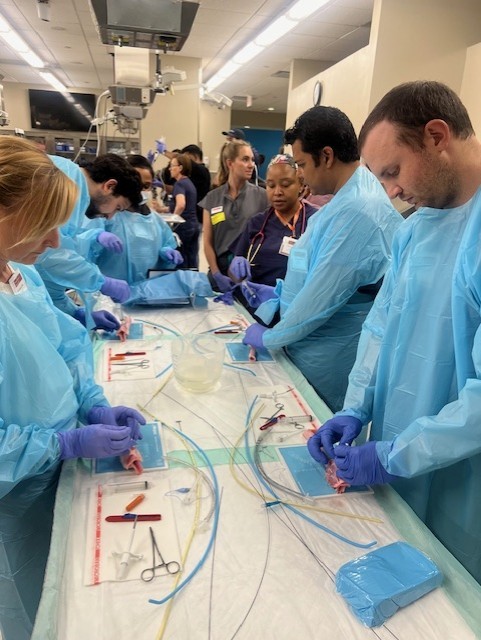
The ICU is a highly collaborative space. I regularly interact with medical students, pediatric residents, and other fellows, which makes for a dynamic and engaging learning atmosphere. The faculty and staff are exceptionally friendly, approachable, and genuinely enjoy teaching. There are abundant hands-on opportunities, including airway management, vascular access, and other procedures, for those interested.
After rounds, fellows are typically free to finish the day unless they choose to stay for procedures or further involvement in patient care. There are no night shifts or call obligations, which allows for a great balance between learning and personal time.
Overall, the Pediatric ICU rotation is an outstanding experience; high-acuity, supportive, and highly customizable to your goals. Whether you are exploring an interest in critical care or just want strong exposure in a collegial environment, this rotation offers something for everyone.
Pediatric Pain Management
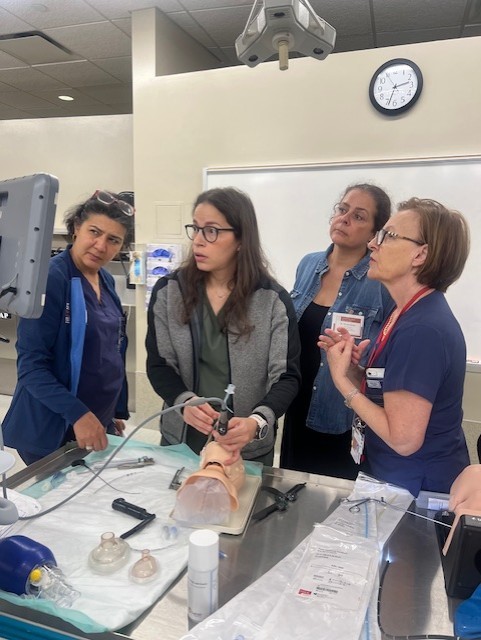
The pediatric acute pain service rotation taught me how to manage acute pain patients and practice regional and neuraxial anesthesia in infants and children. The week before my rotation, I received a packet with helpful information about the rotation, including goals and objectives, acute pain and regional lectures, algorithms for managing different types of pain, as well as relevant articles to review.
On the first day of my rotation, I received a full orientation on what to expect during the rotation. We reviewed everything in my acute pain packet including the lectures which taught me about different nerve blocks in children and pain medication uses and dosing. I learned how to access our patient pain list and write pain notes. Last, we reviewed the operating room (OR) cases for the next day, and I chose regional blocks that I was interested in performing (an epidural in a neonate undergoing an exploratory laparotomy, a sphenopalatine ganglion nerve block in a patient undergoing a Le Fort osteotomy, and an ultrasound guided caudal block in an infant for distal hypospadias repair). I discussed these blocks with the assigned attendings to prepare for the next day. I learned about important labs and questions to ask prior placing nerve blocks on pediatric patients.
On day two, after obtaining consent and setting up for the blocks, I helped start the cases and performed the blocks while the patients were under general anesthesia. I got to place a stimulating epidural catheter for the first time and confirmed placement by visualizing the tip of the catheter on x-ray. I learned how to bolus and run an epidural ropivacaine infusion in a neonate. After all the blocks were done, I sat down with my attending and the acute pain nurse in the doctor’s lounge, and we ran the list over coffee and breakfast. We also discussed other potential blocks that I could do throughout the day, so that we could plan accordingly. Next, we rounded on the pain patients. I learned how to assess pain in all age groups and formulate appropriate pain management plans. I met several pediatric nurses and was amazed at how kind, nice, and involved the nurses were during our discussions over mutual patients. During our rounds we received a new consult on a sickle cell patient in an acute pain crisis. After seeing the patient, I learned how to start and manage a patient-controlled analgesic (PCA) pump on a pediatric patient. Our last consult for the day, was a toddler who sustained a hot soup burn. I learned how the burn team manages these patients, as well as how our pain management algorithm is used to help control pain during bedside dressing changes. Prior to leaving for the day, I ran the OR cases for the next day with my attending, and mapped out a regional plan, so as to maximize the number of blocks that I would get to perform. There were usually lots of regional options for first case starts, so I had to pick and choose the most desirable blocks.
The next day after morning blocks and prerounds were completed, we went to check on our epidural baby. I learned how to assess for pain in a neonate with an epidural, as well as assess the epidural site. Each patient who had received nerve blocks the day before did great with little to no prn pain medication needed overnight.
Throughout the first week, I learned how to transition patients off of both an epidural and a PCA pump. I really enjoyed how the acute pain service takes a patient full circle from the preoperative area to discharge. I also learned how to manage medication side effects, such as pruritus, nausea, and constipation. I learned about treatment of neuropathic pain. There were a couple of light days where we finished early. Those days my attending let me leave early to study and rest.
My month on the pediatric acute pain service taught me so much about pain in all age groups. I feel comfortable coming up with a pain plan in multiple scenarios. My regional anesthesia skills greatly improved with lots of practice using ultrasound guided techniques. Overall, my pain month was a great experience and equipped me with the tools and confidence needed to manage acute pain in infants and children.