Obstetric Anesthesia Fellowship
The Department of Anesthesiology, McGovern Medical School at the University of Texas Health Science Center at Houston (UTHealth), has received initial accreditation from the Accreditation Council for Graduate Medical Education (ACGME) for an Obstetric Anesthesia Fellowship Program. The UTHealth System and McGovern Medical School are located in the Texas Medical Center (TMC)—the world’s largest medical complex—and offer invaluable opportunities for an obstetric anesthesia fellow to further their training.
We are currently seeking qualified fellowship applicants to fill two approved positions.
If you are interested, please contact Dr. Kristin Falce, MD, Director of the Obstetric Anesthesia Fellowship Program at [email protected]
Maternal mortality has been steadily on the rise since the late 20th century. Increasing cases of cardiovascular disease, including congenital heart disease, cardiomyopathy, and congestive heart failure, are the leading cause of maternal mortality in Western countries1. Memorial Hermann Hospital—TMC, our primary private hospital, has approximately 5,000 deliveries/year (mostly insured patients), and Harris Health System’s Lyndon B. Johnson Hospital, our county hospital, has around 2,000 deliveries/year. Between the two clinical locations more than 60% are high-risk parturients. Recently, our obstetric service received accreditation as a Level IV—the highest level of maternal care—which requires a, “Board-certified anesthesiologist with obstetric anesthesia fellowship training or experience in obstetric anesthesia physically present at all times2.” The future is an integrated obstetric critical care team with participation from obstetric anesthesiologists. Currently our division encompasses 10 OB anesthesia trained physicians.
We have multiple faculty who are skilled anesthesiologists and intensivists prepared to train our fellows in Point-of-Care ultrasound-TEE; regional anesthesia techniques; and a state-of-the-art acute pain service. There are also exciting opportunities to participate in simulation, fetal center cases, and to collaborate with the Maternal Fetal Medicine team in safety rounds, and a variety of multidisciplinary meetings, conferences, and joint research.
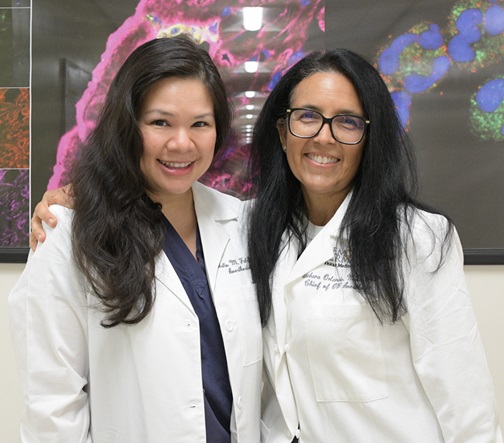
Under the leadership of the department chairman, Dr. Holger K. Eltzschig, MD, PhD, a preeminent researcher in organ injury and perioperative medicine, we also have an ongoing vibrant and cutting edge perioperative research program to study acute kidney injury in pregnant women. Additionally, there are several clinical research projects under development. Dr. Maya Suresh, MD, former President of the Society for Obstetric Anesthesia and Perinatology (SOAP), former President of the Society for Airway Management and lead editor of Shnider and Levinson Anesthesia for Obstetrics, 5th edition spearheaded the creation of the fellowship program and the accreditation of our division as a SOAP Center of Excellence. Our new Division Chief of Obstetric Anesthesia Dr Barbara Orlando, MD, PhD, is continuing the effort initiated by Dr Suresh to increase research involvement and participation in various efforts including maternal safety. Division Chief of Obstetric Anesthesia is part of the fellowship program. Our fellows can anticipate completing their year of training with not only a rich body of experience to enhance their armamentarium of clinical and research skills, knowledge, and confidence needed while caring for any high risk or critically ill obstetric patient, but also opportunities to participate in ongoing research and to present at national conferences.
-
Kuklina E, Callaghan W. Chronic heart disease and severe obstetric morbidity among hospitalisations for pregnancy in the USA: 1995-2006. 2011 Feb;118(3):345-52.
-
ACOG Levels of maternal care. Obstetrics & Gynecology: August 2019 – Volume 134 – Issue 2 – p 425